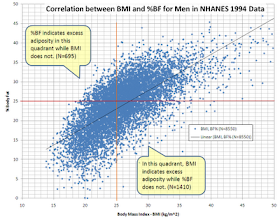
The graph below (from Wikipedia) plots body fat percentage (BF) against body mass index (BMI) for men. The data is a bit old: 1994. The top-left quadrant refers to men with BF greater than 25 percent and BMI lower than 25. A man with a BF greater than 25 has crossed into obese territory, even though a BMI lower than 25 would suggest that he is not even overweight. These folks are what we could call skinny-fat men.
The data is from the National Health and Nutrition Examination Survey (NHANES), so it is from the USA only. Interesting that even though this data is from 1994, we already could find quite a few men with more than 25 percent BF and a BMI of around 20. One example of this would be a man who is 5’11’’, weighing 145 lbs, and who would be technically obese!
About 8 percent of the entire sample of men used as a basis for the plot fell into the area defined by the top-left quadrant – the skinny-fat men. (That quadrant is one in which the BMI measure is quite deceiving; another is the bottom-right quadrant.) Most of us would be tempted to conclude that all of these men were sick or on the path to becoming so. But we do not know this for sure. On the standard American diet, I think it is a reasonably good guess that these skinny-fat men would not fare very well.
What is most interesting for me regarding this data, which definitely has some measurement error built in (e.g., zero BF), is that it suggests that the percentage of skinny-fat men in the general population is surprisingly high. (And this seems to be the case for women as well.) Almost too high to characterize being skinny-fat as a disease per se, much less a genetic disease. Genetic diseases tend to be rarer.
In populations under significant natural selection pressure, which does not include modern humans living in developed countries, genetic diseases tend to be wiped out by evolution. (The unfortunate reality is that modern medicine helps these diseases spread, although quite slowly.) Moreover, the prevalence of diabetes in the population was not as high as 8 percent in 1994, and is not that high today either; although it tends to be concentrated in some areas and cluster with obesity as defined based on both BF and BMI.
And again, who knows, maybe these folks (the skinny-fat men) were not even the least healthy in the whole sample, as one may be tempted to conclude.
Maybe being skinny-fat is a trait, passed on across generations, not a disease. Maybe such a trait was useful at some point in the not so distant past to some of our ancestors, but leads to degenerative diseases in the context of a typical Western diet. Long-living Asians with low BMI tend to gravitate more toward the skinny-fat quadrant than many of their non-Asian counterparts. That is, long-living Asians generally tend have higher BF percentage at the same BMI (see a discussion about the Okinawans on this post).
Evolution is a deceptively simple process, which can lead to very odd results.
This “trait-not-disease” idea may sound like semantics, but it has major implications. It would mean that many of the folks who are currently seen as diseased or disease-prone, are in fact simply “different”. At a point in time in our past, under a unique set of circumstances, they might have been the ones who would have survived. The ones who would have been perceived as healthier than average.
Monday, August 29, 2011
Monday, August 22, 2011
Refined carbohydrate-rich foods, palatability, glycemic load, and the Paleo movement
A great deal of discussion has been going on recently revolving around the so-called “carbohydrate hypothesis of obesity”. I will use the acronym CHO to refer to this hypothesis. This acronym is often used to refer to carbohydrates in nutrition research; I hope this will not cause confusion.
The CHO could be summarized as this: a person consumes foods with “easily digestible” carbohydrates, those carbohydrates raise insulin levels abnormally, the abnormally high insulin levels drive too much fat into body fat cells and keep it there, this causes hunger as not enough fat is released from fat cells for use as energy, this hunger drives the consumption of more foods with “easily digestible” carbohydrates, and so on.
It is posited as a feedback-loop process that causes serious problems over a period of years. The term “easily digestible” is within quotes for emphasis. If it is taken to mean “refined”, which is still a bit vague, there is a good amount of epidemiological evidence in support of the CHO. If it is taken to mean simply “easily digestible”, as in potatoes and rice (which is technically a refined food, but a rather benign one), there is a lot of evidence against it. Even from an unbiased (hopefully) look at county-level data in the China Study.
Another hypothesis that has been around for a long time and that has been revived recently, which we could call the “palatability hypothesis”, is a competing hypothesis. It is an interesting and intriguing hypothesis, at least at first glance. There seems to be some truth to this hypothesis. The idea here is that we have not evolved mechanisms to deal with highly palatable foods, and thus end up overeating them. Therefore we should go in the opposite direction, and place emphasis on foods that are not very palatable to reach our optimal weight. You might think that to test this hypothesis it would be enough to find out if this diet works: “Eat something … if it tastes good, spit it out!”
But it is not so simple. To test this palatability hypothesis one could try to measure the palatability of foods, and see if it is correlated with consumption. The problem is that the formulations I have seen of the palatability hypothesis treat the palatability construct as static, when in fact it is dynamic – very dynamic. The perception of the reward associated with a specific food changes depending on a number of factors.
For example, we cannot assign a palatability score to a food without considering the particular state in which the individual who eats the food is. That state is defined by a number of factors, including physiological and psychological ones, which vary a lot across individuals and even across different points in time for the same individual. For someone who is hungry after a 20 h fast, for instance, the perceived reward associated with a food will go up significantly compared to the same person in the fed state.
Regarding the CHO, it seems very clear that refined carbohydrate-rich foods in general, particularly the highly modified ones, disrupt normal biological mechanisms that regulate hunger. Perceived food reward, or palatability, is a function of hunger. Abnormal glucose and insulin responses appear to be at the core of this phenomenon. There are undoubtedly many other factors at play as well. But, as you can see, there is a major overlap between the CHO and the palatability hypothesis. Refined carbohydrate-rich foods generally have higher palatability than natural foods in general. Humans are good engineers.
One meme that seems to be forming recently on the Internetz is that the CHO is incompatible with data from healthy isolated groups that consume a lot of carbohydrates, which are sometimes presented as alternative models of life in the Paleolithic. But in fact among influential proponents of the CHO are the intellectual founders of the Paleolithic dieting movement. Including folks who studied native diets high in carbohydrates, and found their users to be very healthy (e.g., the Kitavans). One thing that these intellectual founders did though was to clearly frame the CHO in terms of refined carbohydrate-rich foods.
Natural carbohydrate-rich foods are clearly distinguished from refined ones based on one key attribute; not the only one, but a very important one nonetheless. That attribute is their glycemic load (GL). I am using the term “natural” here as roughly synonymous with “unrefined” or “whole”. Although they are often confused, the GL is not the same as the glycemic index (GI). The GI is a measure of the effect of carbohydrate intake on blood sugar levels. Glucose is the reference; it has a GI of 100.
The GL provides a better way of predicting total blood sugar response, in terms of “area under the curve”, based on both the type and quantity of carbohydrate in a specific food. Area under the curve is ultimately what really matters; a pointed but brief spike may not have much of a metabolic effect. Insulin response is highly correlated with blood sugar response in terms of area under the curve. The GL is calculated through the following formula:
GL = (GI x the amount of available carbohydrate in grams) / 100
The GL of a food is also dynamic, but its range of variation is small enough in normoglycemic individuals so that it can be treated as a relatively static number. (Still, the reference are normoglycemic individuals.) One of the main differences between refined and natural carbohydrate-rich foods is the much higher GL of industrial carbohydrate-rich foods, and this is not affected by slight variations in GL and GI depending on an individual’s state. The table below illustrates this difference.
Looking back at the environment of our evolutionary adaptation (EEA), which was not static either, this situation becomes analogous to that of vitamin D deficiency today. A few minutes of sun exposure stimulate the production of 10,000 IU of vitamin D, whereas food fortification in the standard American diet normally provides less than 500 IU. The difference is large. So is the difference in GL of natural and refined carbohydrate-rich foods.
And what are the immediate consequences of that difference in GL values? They are abnormally elevated blood sugar and insulin levels after meals containing refined carbohydrate-rich foods. (Incidentally, the GL happens to be relatively low for the rice preparations consumed by Asian populations who seem to do well on rice-based diets.) Abnormal levels of other hormones, in a chronic fashion, come later, after many years consuming those foods. These hormones include adiponectin, leptin, and tumor necrosis factor. The authors of the article from which the table above was taken note that:
Who are the authors of this article? They are Loren Cordain, S. Boyd Eaton, Anthony Sebastian, Neil Mann, Staffan Lindeberg, Bruce A. Watkins, James H O’Keefe, and Janette Brand-Miller. The paper is titled “Origins and evolution of the Western diet: Health implications for the 21st century”. A full-text PDF is available here. For most of these authors, this article is their most widely cited publication so far, and it is piling up citations as I write. This means that not only members of the general public have been reading it, but that professional researchers have been reading it as well, and citing it in their own research publications.
In summary, the CHO and the palatability hypothesis overlap, and the overlap is not trivial. But the palatability hypothesis is more difficult to test. As Karl Popper noted, a good hypothesis is a testable hypothesis. Eating natural foods will make an enormous difference for the better in your health if you are coming from the standard American diet, and you can justify this statement based on the CHO, the palatability hypothesis, or even a few others – e.g., a nutrient density hypothesis, which would be closer to Weston Price's views. Even if you eat only plant-based natural foods, which I cannot fully recommend based on data I’ve reviewed on this blog, you will be better off.
The CHO could be summarized as this: a person consumes foods with “easily digestible” carbohydrates, those carbohydrates raise insulin levels abnormally, the abnormally high insulin levels drive too much fat into body fat cells and keep it there, this causes hunger as not enough fat is released from fat cells for use as energy, this hunger drives the consumption of more foods with “easily digestible” carbohydrates, and so on.
It is posited as a feedback-loop process that causes serious problems over a period of years. The term “easily digestible” is within quotes for emphasis. If it is taken to mean “refined”, which is still a bit vague, there is a good amount of epidemiological evidence in support of the CHO. If it is taken to mean simply “easily digestible”, as in potatoes and rice (which is technically a refined food, but a rather benign one), there is a lot of evidence against it. Even from an unbiased (hopefully) look at county-level data in the China Study.
Another hypothesis that has been around for a long time and that has been revived recently, which we could call the “palatability hypothesis”, is a competing hypothesis. It is an interesting and intriguing hypothesis, at least at first glance. There seems to be some truth to this hypothesis. The idea here is that we have not evolved mechanisms to deal with highly palatable foods, and thus end up overeating them. Therefore we should go in the opposite direction, and place emphasis on foods that are not very palatable to reach our optimal weight. You might think that to test this hypothesis it would be enough to find out if this diet works: “Eat something … if it tastes good, spit it out!”
But it is not so simple. To test this palatability hypothesis one could try to measure the palatability of foods, and see if it is correlated with consumption. The problem is that the formulations I have seen of the palatability hypothesis treat the palatability construct as static, when in fact it is dynamic – very dynamic. The perception of the reward associated with a specific food changes depending on a number of factors.
For example, we cannot assign a palatability score to a food without considering the particular state in which the individual who eats the food is. That state is defined by a number of factors, including physiological and psychological ones, which vary a lot across individuals and even across different points in time for the same individual. For someone who is hungry after a 20 h fast, for instance, the perceived reward associated with a food will go up significantly compared to the same person in the fed state.
Regarding the CHO, it seems very clear that refined carbohydrate-rich foods in general, particularly the highly modified ones, disrupt normal biological mechanisms that regulate hunger. Perceived food reward, or palatability, is a function of hunger. Abnormal glucose and insulin responses appear to be at the core of this phenomenon. There are undoubtedly many other factors at play as well. But, as you can see, there is a major overlap between the CHO and the palatability hypothesis. Refined carbohydrate-rich foods generally have higher palatability than natural foods in general. Humans are good engineers.
One meme that seems to be forming recently on the Internetz is that the CHO is incompatible with data from healthy isolated groups that consume a lot of carbohydrates, which are sometimes presented as alternative models of life in the Paleolithic. But in fact among influential proponents of the CHO are the intellectual founders of the Paleolithic dieting movement. Including folks who studied native diets high in carbohydrates, and found their users to be very healthy (e.g., the Kitavans). One thing that these intellectual founders did though was to clearly frame the CHO in terms of refined carbohydrate-rich foods.
Natural carbohydrate-rich foods are clearly distinguished from refined ones based on one key attribute; not the only one, but a very important one nonetheless. That attribute is their glycemic load (GL). I am using the term “natural” here as roughly synonymous with “unrefined” or “whole”. Although they are often confused, the GL is not the same as the glycemic index (GI). The GI is a measure of the effect of carbohydrate intake on blood sugar levels. Glucose is the reference; it has a GI of 100.
The GL provides a better way of predicting total blood sugar response, in terms of “area under the curve”, based on both the type and quantity of carbohydrate in a specific food. Area under the curve is ultimately what really matters; a pointed but brief spike may not have much of a metabolic effect. Insulin response is highly correlated with blood sugar response in terms of area under the curve. The GL is calculated through the following formula:
GL = (GI x the amount of available carbohydrate in grams) / 100
The GL of a food is also dynamic, but its range of variation is small enough in normoglycemic individuals so that it can be treated as a relatively static number. (Still, the reference are normoglycemic individuals.) One of the main differences between refined and natural carbohydrate-rich foods is the much higher GL of industrial carbohydrate-rich foods, and this is not affected by slight variations in GL and GI depending on an individual’s state. The table below illustrates this difference.
Looking back at the environment of our evolutionary adaptation (EEA), which was not static either, this situation becomes analogous to that of vitamin D deficiency today. A few minutes of sun exposure stimulate the production of 10,000 IU of vitamin D, whereas food fortification in the standard American diet normally provides less than 500 IU. The difference is large. So is the difference in GL of natural and refined carbohydrate-rich foods.
And what are the immediate consequences of that difference in GL values? They are abnormally elevated blood sugar and insulin levels after meals containing refined carbohydrate-rich foods. (Incidentally, the GL happens to be relatively low for the rice preparations consumed by Asian populations who seem to do well on rice-based diets.) Abnormal levels of other hormones, in a chronic fashion, come later, after many years consuming those foods. These hormones include adiponectin, leptin, and tumor necrosis factor. The authors of the article from which the table above was taken note that:
Within the past 20 y, substantial evidence has accumulated showing that long term consumption of high glycemic load carbohydrates can adversely affect metabolism and health. Specifically, chronic hyperglycemia and hyperinsulinemia induced by high glycemic load carbohydrates may elicit a number of hormonal and physiologic changes that promote insulin resistance. Chronic hyperinsulinemia represents the primary metabolic defect in the metabolic syndrome.
Who are the authors of this article? They are Loren Cordain, S. Boyd Eaton, Anthony Sebastian, Neil Mann, Staffan Lindeberg, Bruce A. Watkins, James H O’Keefe, and Janette Brand-Miller. The paper is titled “Origins and evolution of the Western diet: Health implications for the 21st century”. A full-text PDF is available here. For most of these authors, this article is their most widely cited publication so far, and it is piling up citations as I write. This means that not only members of the general public have been reading it, but that professional researchers have been reading it as well, and citing it in their own research publications.
In summary, the CHO and the palatability hypothesis overlap, and the overlap is not trivial. But the palatability hypothesis is more difficult to test. As Karl Popper noted, a good hypothesis is a testable hypothesis. Eating natural foods will make an enormous difference for the better in your health if you are coming from the standard American diet, and you can justify this statement based on the CHO, the palatability hypothesis, or even a few others – e.g., a nutrient density hypothesis, which would be closer to Weston Price's views. Even if you eat only plant-based natural foods, which I cannot fully recommend based on data I’ve reviewed on this blog, you will be better off.
Monday, August 15, 2011
Book review: Sugar Nation
Jeff O’Connell is the Editor-in-Chief for Bodybuilding.com, a former executive writer for Men’s Health, and former Editor-in-Chief of Muscle & Fitness. He is also the author of a few bestselling books on fitness.
It is obvious that Jeff is someone who can write, and this comes across very clearly in his new book, Sugar Nation.
Now, with a title like this, Sugar Nation, I was expecting a book discussing trends of sugar consumption in the USA, and the related trends in various degenerative diseases. So when I started reading the book I was slightly put off by what seemed to be a book about a very personal journey, written in the first person by the author.
Yet, after reading it for a while I was hooked, and literally could not put the book down. Jeff has managed to write something of a page-turner, combining a harrowing personal account with carefully researched scientific information, about a relatively rare form of type 2 diabetes.
Jeff has a genetic propensity to insulin resistance, just like his father did. What makes Jeff’s case a little unusual is that Jeff is thin, and apparently has difficulty gaining weight. The most common type of diabetes is type 2, and most of those who develop type 2 diabetes do so via the metabolic syndrome. Typically this involves becoming obese or overweight before getting diagnosed as a diabetic.
In fact, in a thin person who is insulin resistant it seems that body fat cells become resistant to the normal actions of insulin much sooner than in the obese. This essentially means that they start rejecting fat. This is a problem, because fat should either be stored in fat cells (adipocytes) or used for energy; as opposed to being deposited in other tissues or remaining in circulation. Apparently this makes it even more difficult for them to control glucose levels once insulin resistance sets in; there is no “cushion”, so to speak.
Still, Jeff appears to believe that his case was that of a skinny-fat person, where body fat percentage is a lot higher than expected based on a low body mass index, and where excess visceral fat is a main culprit. In fact, Jeff seems to think that most cases of thin folks who developed type 2 diabetes are like this, as they follow the metabolic syndrome progression pattern. Fasting triglycerides go up and HDL cholesterol goes down, among other things, but in a skinny-fat body.
Somewhat predictably, what Jeff found out is that, in his case, adopting a low carbohydrate diet made an enormous difference. In fact, it made the difference between having a fairly normal life versus constantly suffering through hypoglycemic episodes. And, at the stage in which Jeff caught the problem, he did not have to avoid all natural carbohydrate-rich foods, not even things like apples. (He had to control portions though.) It is the refined carbohydrate-rich foods that were the problem for him.
I must say that I disagree with a few of the statements in the book. For example, the author seems to believe that excess saturated fat and salt may be quite unhealthy. I think that foods rich in refined carbohydrates and sugars are much more of a problem; cut them out and often excess saturated fat and salt either cease to be a problem, or become healthy. Jeff doesn’t seem to think that excess omega-6 fats can also cause diabetes; I believe the opposite to be true, via a pro-inflammatory path.
Still, this is a great book on so many levels. Jeff meticulously records his experience dealing with doctors, most of whom seem to be clueless as to what to do to prevent the damage that is caused by abnormally high glucose levels. This happens even though diabetes is those doctors’ main area of expertise. He talks about himself with complete abandon, and manages to mix that up with quite a lot of relevant research on diabetes. He gives us an insider’s view of the professional bodybuilding culture, including its use of insulin injections. His description of the Amish is very interesting and somewhat surprising.
For these reasons and a few others, I think this is a great book, and highly recommend it!
(Source: Bodybuilding.com)
It is obvious that Jeff is someone who can write, and this comes across very clearly in his new book, Sugar Nation.
Now, with a title like this, Sugar Nation, I was expecting a book discussing trends of sugar consumption in the USA, and the related trends in various degenerative diseases. So when I started reading the book I was slightly put off by what seemed to be a book about a very personal journey, written in the first person by the author.
Yet, after reading it for a while I was hooked, and literally could not put the book down. Jeff has managed to write something of a page-turner, combining a harrowing personal account with carefully researched scientific information, about a relatively rare form of type 2 diabetes.
Jeff has a genetic propensity to insulin resistance, just like his father did. What makes Jeff’s case a little unusual is that Jeff is thin, and apparently has difficulty gaining weight. The most common type of diabetes is type 2, and most of those who develop type 2 diabetes do so via the metabolic syndrome. Typically this involves becoming obese or overweight before getting diagnosed as a diabetic.
In fact, in a thin person who is insulin resistant it seems that body fat cells become resistant to the normal actions of insulin much sooner than in the obese. This essentially means that they start rejecting fat. This is a problem, because fat should either be stored in fat cells (adipocytes) or used for energy; as opposed to being deposited in other tissues or remaining in circulation. Apparently this makes it even more difficult for them to control glucose levels once insulin resistance sets in; there is no “cushion”, so to speak.
Still, Jeff appears to believe that his case was that of a skinny-fat person, where body fat percentage is a lot higher than expected based on a low body mass index, and where excess visceral fat is a main culprit. In fact, Jeff seems to think that most cases of thin folks who developed type 2 diabetes are like this, as they follow the metabolic syndrome progression pattern. Fasting triglycerides go up and HDL cholesterol goes down, among other things, but in a skinny-fat body.
Somewhat predictably, what Jeff found out is that, in his case, adopting a low carbohydrate diet made an enormous difference. In fact, it made the difference between having a fairly normal life versus constantly suffering through hypoglycemic episodes. And, at the stage in which Jeff caught the problem, he did not have to avoid all natural carbohydrate-rich foods, not even things like apples. (He had to control portions though.) It is the refined carbohydrate-rich foods that were the problem for him.
I must say that I disagree with a few of the statements in the book. For example, the author seems to believe that excess saturated fat and salt may be quite unhealthy. I think that foods rich in refined carbohydrates and sugars are much more of a problem; cut them out and often excess saturated fat and salt either cease to be a problem, or become healthy. Jeff doesn’t seem to think that excess omega-6 fats can also cause diabetes; I believe the opposite to be true, via a pro-inflammatory path.
Still, this is a great book on so many levels. Jeff meticulously records his experience dealing with doctors, most of whom seem to be clueless as to what to do to prevent the damage that is caused by abnormally high glucose levels. This happens even though diabetes is those doctors’ main area of expertise. He talks about himself with complete abandon, and manages to mix that up with quite a lot of relevant research on diabetes. He gives us an insider’s view of the professional bodybuilding culture, including its use of insulin injections. His description of the Amish is very interesting and somewhat surprising.
For these reasons and a few others, I think this is a great book, and highly recommend it!
Monday, August 8, 2011
Potassium deficiency in low carbohydrate dieting: High protein and fat alternatives that do not involve supplementation
It is often pointed out, at least anecdotally, that potassium deficiency is common among low carbohydrate dieters. Potassium deficiency can lead to a number of unpleasant symptoms and health problems. This micronutrient is present in small quantities in meat and seafood; main sources are plant foods.
A while ago this has gotten me thinking and asking myself: what about isolated hunter-gatherers that seem to have thrived consuming mostly carnivorous diets with little potassium, such as various Native American tribes?
Another thought came to mind, which is that animal protein seems to be associated with increased bone mineralization, even when calcium intake is low. That seems to be due to animal protein being associated with increased absorption of calcium and other minerals that make up bone tissue.
Maybe animal protein intake is also associated with increased potassium absorption. If this is true, what could be the possible mechanism?
As it turns out, there is one possible and somewhat surprising connection, insulin seems to promote cell uptake of potassium. This is an argument made many years ago by Clausen and Kohn, and further discussed more recently by Benziane and Chibalin. See also this recent commentary by Clausen.
Protein is the only macronutrient that normally causes transient insulin elevation without any glucose response. And the insulin response to protein is nowhere near that associated with refined carbohydrate-rich foods. It is much lower, analogous to the response to natural carbohydrate-rich foods.
A very low carbohydrate diet with more animal protein, and less fat, would induce insulin responses after meals, possibly helping with the absorption of potassium, even if potassium intake were rather limited. Primarily carnivorous diets, like those of some traditional Native American groups, would fit the bill.
Also, a low carbohydrate diet with emphasis on fat, but that was not so low in carbohydrates from certain sources, would probably achieve the same effect. This latter sounds like Kwaśniewski’s Optimal Diet, where people are encouraged to eat a lot more fat than protein, but also a small amount of carbohydrates (e.g., 50-100 g/d) from things like potatoes.
Kwaśniewski’s suggestions may sound counterintuitive sometimes. But, as it turns out, potatoes are good sources of potassium. One potato may not be a lot, but that potato will also increase insulin levels, bringing potassium intake up at the cell level.
A while ago this has gotten me thinking and asking myself: what about isolated hunter-gatherers that seem to have thrived consuming mostly carnivorous diets with little potassium, such as various Native American tribes?
Another thought came to mind, which is that animal protein seems to be associated with increased bone mineralization, even when calcium intake is low. That seems to be due to animal protein being associated with increased absorption of calcium and other minerals that make up bone tissue.
Maybe animal protein intake is also associated with increased potassium absorption. If this is true, what could be the possible mechanism?
As it turns out, there is one possible and somewhat surprising connection, insulin seems to promote cell uptake of potassium. This is an argument made many years ago by Clausen and Kohn, and further discussed more recently by Benziane and Chibalin. See also this recent commentary by Clausen.
Protein is the only macronutrient that normally causes transient insulin elevation without any glucose response. And the insulin response to protein is nowhere near that associated with refined carbohydrate-rich foods. It is much lower, analogous to the response to natural carbohydrate-rich foods.
A very low carbohydrate diet with more animal protein, and less fat, would induce insulin responses after meals, possibly helping with the absorption of potassium, even if potassium intake were rather limited. Primarily carnivorous diets, like those of some traditional Native American groups, would fit the bill.
Also, a low carbohydrate diet with emphasis on fat, but that was not so low in carbohydrates from certain sources, would probably achieve the same effect. This latter sounds like Kwaśniewski’s Optimal Diet, where people are encouraged to eat a lot more fat than protein, but also a small amount of carbohydrates (e.g., 50-100 g/d) from things like potatoes.
Kwaśniewski’s suggestions may sound counterintuitive sometimes. But, as it turns out, potatoes are good sources of potassium. One potato may not be a lot, but that potato will also increase insulin levels, bringing potassium intake up at the cell level.
Monday, August 1, 2011
There is no doubt that abnormally elevated insulin is associated with body fat accumulation
For as long as diets existed there have been influential proponents, or believers, who at some point had what they thought were epiphanies. From that point forward, they disavowed the diets that they formally endorsed. Low carbohydrate dieting seems to be in this situation now. Among other things, it has been recently “discovered” that the idea that insulin drives fat into body fat cells is “wrong”.
Based on some of the comments I have been receiving lately, apparently a few readers think that I am one of those “enlightened”. If you are interested in what I have been eating, for quite some time now, just click on the link at the top of this blog that refers to my transformation. It is essentially high in all macronutrients on days that I exercise, and low in carbohydrates and calories on days that I don’t. It is a cyclic approach that works for me; calorie surpluses on some days and calorie deficits on other days.
But let me set the record straight regarding what I think: there is no doubt that insulin is associated with body fat accumulation. I was told that an influential health blogger (whom I respect a lot) denied this recently, going to the extreme of saying that no professional metabolism or endocrinology researcher believes in it, but I couldn’t find any evidence of that statement. It is not hard at all to find professional metabolism and endocrinology researchers who have asserted that insulin is associated with body fat accumulation, based on very reliable evidence. Actually, this is Biochemistry 101.
What I think is truly unclear is whether insulin spikes associated with carbohydrate-rich foods in general are the cause of obesity. This idea is, indeed, probably wrong given the evidence we have from various human populations whose members consume plenty of non-industrialized carbohydrate-rich foods. On a related note, I particularly disagree with the notion that the pancreas gets tired over time due to having to secrete insulin in bursts, which seems to also be one of the foundations on which many low carbohydrate diet varieties rest.
As with almost everything related to health, the role of insulin in body fat gain is complex, and part of that complexity is due to the nonlinear relationship between body fat gain and postprandial insulin release. Industrial carbohydrate-rich foods have a much higher glycemic load than natural carbohydrate-rich foods, even though their glycemic index may be the same in some cases. In other words, the quantity of easily digestible carbohydrates per gram is much higher in industrial carbohydrate-rich foods.
In normoglycemic folks, this leads to an abnormally elevated insulin response, among other hormonal responses. For example, circulating growth hormone, which promotes body fat loss, is inversely correlated with circulating insulin. Insulin drives fat, typically from dietary sources of fat, into adipocytes. That fat may also come from excess carbohydrates, packaged into VLDL particles.
Under normal circumstances, that would be fine, since our body is designed to store fat and release it as needed. But the abnormal insulin response elicited by industrial carbohydrate-rich foods, together with other hormonal responses, leads to a little more body fat accumulation, and for longer, than it should. And I’m talking here about people without any metabolic damage. Saturated and monounsaturated fats are healthy when eaten, but when they are stored as excess body fat, they become pro-inflammatory.
Body fat is like an organ, secreting many hormones into the bloodstream, several of which are pro-inflammatory. One of those pro-inflammatory hormones, which I believe is closely linked with many diseases of civilization, is tumor necrosis factor. (The acronym is now TNF. Apparently the “-alpha” after its name and acronym has been dropped recently.) Dietary fat, particularly saturated fat, seems to be anti-inflammatory. In other words, body fat accumulation is the problem. You only need 30 g/d of excess body fat accumulation to gain around 24 lbs of fat per year. Over three years, that will add up to over 70 lbs of body fat.
In my view, ultimately it is excess inflammation (which is, in essence, a vascular response) that is at the source of most of the diseases of civilization.
That is where the nonlinearity comes in. Insulin is healthy up to a point. Beyond that, it starts causing health problems, over time. And one of the main mechanisms by which it does so is via excessive body fat accumulation, with different damage threshold levels for different people. Insulin may decrease appetite as it goes up, but it increases it if goes down too much. If it goes up abnormally, typically it will go down too much. As it reaches a trough it induces hypoglycemia, even if mildly.
Take a look at the graph below, from this post showing the glucose variations in normoglycemic individuals. There is a lot of variation among different individuals, but it is clear that the magnitude of the hypoglycemic dips is inversely correlated with the magnitude of the glucose spikes. That inverse correlation is due primarily to the effect of insulin. Under normal circumstances, a decrease in circulating insulin would promote an increase in free fatty acids in circulation, which would normally have a suppressing effect on hunger in the hours after a meal. But industrial carbohydrate-rich foods lead to increases and decreases in glucose and insulin that are too steep, causing the opposite effect.
You may ask: why do you keep talking about industrial carbohydrate-rich foods? Why not talk about industrial protein- or fat-rich foods as well? The reason is that the food industry has not been very successful at producing industrial protein- or fat-rich foods that are palatable without adding a lot of carbohydrate to them.
More often than not they need enough carbohydrate added in the form of sugar to become truly addictive.
Based on some of the comments I have been receiving lately, apparently a few readers think that I am one of those “enlightened”. If you are interested in what I have been eating, for quite some time now, just click on the link at the top of this blog that refers to my transformation. It is essentially high in all macronutrients on days that I exercise, and low in carbohydrates and calories on days that I don’t. It is a cyclic approach that works for me; calorie surpluses on some days and calorie deficits on other days.
But let me set the record straight regarding what I think: there is no doubt that insulin is associated with body fat accumulation. I was told that an influential health blogger (whom I respect a lot) denied this recently, going to the extreme of saying that no professional metabolism or endocrinology researcher believes in it, but I couldn’t find any evidence of that statement. It is not hard at all to find professional metabolism and endocrinology researchers who have asserted that insulin is associated with body fat accumulation, based on very reliable evidence. Actually, this is Biochemistry 101.
What I think is truly unclear is whether insulin spikes associated with carbohydrate-rich foods in general are the cause of obesity. This idea is, indeed, probably wrong given the evidence we have from various human populations whose members consume plenty of non-industrialized carbohydrate-rich foods. On a related note, I particularly disagree with the notion that the pancreas gets tired over time due to having to secrete insulin in bursts, which seems to also be one of the foundations on which many low carbohydrate diet varieties rest.
As with almost everything related to health, the role of insulin in body fat gain is complex, and part of that complexity is due to the nonlinear relationship between body fat gain and postprandial insulin release. Industrial carbohydrate-rich foods have a much higher glycemic load than natural carbohydrate-rich foods, even though their glycemic index may be the same in some cases. In other words, the quantity of easily digestible carbohydrates per gram is much higher in industrial carbohydrate-rich foods.
In normoglycemic folks, this leads to an abnormally elevated insulin response, among other hormonal responses. For example, circulating growth hormone, which promotes body fat loss, is inversely correlated with circulating insulin. Insulin drives fat, typically from dietary sources of fat, into adipocytes. That fat may also come from excess carbohydrates, packaged into VLDL particles.
Under normal circumstances, that would be fine, since our body is designed to store fat and release it as needed. But the abnormal insulin response elicited by industrial carbohydrate-rich foods, together with other hormonal responses, leads to a little more body fat accumulation, and for longer, than it should. And I’m talking here about people without any metabolic damage. Saturated and monounsaturated fats are healthy when eaten, but when they are stored as excess body fat, they become pro-inflammatory.
Body fat is like an organ, secreting many hormones into the bloodstream, several of which are pro-inflammatory. One of those pro-inflammatory hormones, which I believe is closely linked with many diseases of civilization, is tumor necrosis factor. (The acronym is now TNF. Apparently the “-alpha” after its name and acronym has been dropped recently.) Dietary fat, particularly saturated fat, seems to be anti-inflammatory. In other words, body fat accumulation is the problem. You only need 30 g/d of excess body fat accumulation to gain around 24 lbs of fat per year. Over three years, that will add up to over 70 lbs of body fat.
In my view, ultimately it is excess inflammation (which is, in essence, a vascular response) that is at the source of most of the diseases of civilization.
That is where the nonlinearity comes in. Insulin is healthy up to a point. Beyond that, it starts causing health problems, over time. And one of the main mechanisms by which it does so is via excessive body fat accumulation, with different damage threshold levels for different people. Insulin may decrease appetite as it goes up, but it increases it if goes down too much. If it goes up abnormally, typically it will go down too much. As it reaches a trough it induces hypoglycemia, even if mildly.
Take a look at the graph below, from this post showing the glucose variations in normoglycemic individuals. There is a lot of variation among different individuals, but it is clear that the magnitude of the hypoglycemic dips is inversely correlated with the magnitude of the glucose spikes. That inverse correlation is due primarily to the effect of insulin. Under normal circumstances, a decrease in circulating insulin would promote an increase in free fatty acids in circulation, which would normally have a suppressing effect on hunger in the hours after a meal. But industrial carbohydrate-rich foods lead to increases and decreases in glucose and insulin that are too steep, causing the opposite effect.
You may ask: why do you keep talking about industrial carbohydrate-rich foods? Why not talk about industrial protein- or fat-rich foods as well? The reason is that the food industry has not been very successful at producing industrial protein- or fat-rich foods that are palatable without adding a lot of carbohydrate to them.
More often than not they need enough carbohydrate added in the form of sugar to become truly addictive.