I blogged before about the study by David Spence and colleagues, published online in July 2012 in the journal Atherosclerosis (). This study attracted a lot of media attention (e.g., ). The article is titled: “Egg yolk consumption and carotid plaque”. The study argues that “regular consumption of egg yolk should be avoided by persons at risk of cardiovascular disease”. It hints at egg yolks being unhealthy in general, possibly even more so than cigarettes.
I used the numbers in Table 2 of the article (only 5 rows of data, one per quintile; i.e., N=5) to conduct a type of analysis that is rarely if ever conducted in health studies – a moderating effects analysis. A previous blog post summarizes the results of one such analysis using WarpPLS (). It looked into the effect of the number of eggs consumed per week on the association between blood LDL cholesterol and plaque (carotid plaque). The conclusion, which is admittedly tentative due to the small sample (N=5), was that plaque decreased as LDL cholesterol increased with consumption of 2.3 eggs per week or more ().
Recently I ran an analysis on the moderating effect of number of eggs consumed per week on the association between cumulative smoking (measured in “pack years”) and plaque. As it turns out, if you fit a 3D surface to the five data points that you get for these three variables from Table 2 of the article, you end up with a relatively smooth surface. Below is a 3D plot of the 5 data points, followed by a best-fitting 3D surface (developed using an experimental algorithm).
Based on this best-fitting surface you could then generate a contour graph, shown below. The “lines” are called “isolines”. Each isoline refers to plaque values that are constant for a set of eggs per week and cumulative smoking combinations. Next to the isolines are the corresponding plaque values. The first impression is indeed that both egg consumption and smoking are causing plaque buildup, as plaque clearly increases as one moves toward the top-right corner of the graph.
But focus your attention on each individual isoline, one at a time. It is clear that plaque remains constant for increases in cumulative smoking, as long as egg consumption increases. Take for example the isoline that refers to 120 mm2 of plaque area. An increase in cumulative smoking from about 14.5 to 16 pack years leads to no increase in plaque if egg consumption goes up from about 2 to 2.3 eggs per week.
These within-isoline trends, which are fairly stable across isolines (they are all slanted to the right), clearly contradict the idea that eggs cause plaque buildup. So, why does plaque buildup seem to clearly increase with egg consumption? Here is a good reason: egg consumption is very strongly correlated with age, and plaque increases with age. The correlation is a whopping 0.916. And I am not talking about cumulative egg consumption, which the authors also measure, through a variable called “egg-yolk years”. No, I am talking about eggs per week. In this dataset, older folks were eating more eggs, period.
The correlation between plaque and age is even higher: 0.977. Given this, it makes sense to look at individual isolines. This would be analogous to what biostatisticians often call “adjusting for age”, or analyzing the effect of egg consumption on plaque buildup “keeping age constant”. A different technique is to “control for age”; this technique would be preferable had the correlations been lower (say, lower than 0.7), as collinearity levels might have been below acceptable thresholds.
The underlying logic of the “keeping age constant” technique is fairly sound in the face of such a high correlation, which would make “controlling for age” very difficult due to collinearity. When we “keep age constant”, the results point at egg consumption being protective among smokers.
But diehard fans of the idea that eggs are unhealthy could explain the results differently. Maybe egg consumption causes plaque to go up, but smoking has a protective effect. Again taking the isoline that refers to 120 mm2 of plaque area, these diehard fans could say that an increase in egg consumption from 2 to 2.3 eggs per week leads to no increase in plaque if cumulative smoking goes up from about 14.5 to 16 pack years.
Not too long ago I also blogged about a medical case study of a man who ate approximately 25 eggs (20 to 30) per day for over 15 years (probably well over), was almost 90 years old (88) when the case was published in the prestigious The New England Journal of Medicine, and was in surprisingly good health (). This man was not a smoker.
Perhaps if this man smoked 25 cigarettes per day, and ate no eggs, he would be in even better health eh!?
Monday, December 24, 2012
Monday, December 10, 2012
Does tallness cause heart disease? No, but sex does
Popular beliefs about medical issues are sometimes motivated by a statistical phenomenon known as “spurious relationship”, among other names. Two variables X and Y are influenced by a third variable C, which leads to X and Y being correlated and thus the impression that X and Y are causally associated.
Take a look at the table below, which I blogged about in a previous post (). This table shows that there is a strong unadjusted correlation between height and arterial stiffness, a marker of heart disease. The likelihood that the correlation is due to chance is lower than one tenth of a percentage point (P<.001).
Interestingly, the authors of the study even use height as a control variable to narrow down the “true” causes of arterial stiffness (column with adjusted results), assuming that height did indeed influence arterial stiffness and what they found to be a key predictor of arterial stiffness, 2-hour postprandial glucose.
But there is no convincing evidence that height causes heart disease, with exception of pathological extremes – e.g., acromegaly. Extremes tend to influence statistical results somewhat, leading to conflicting conclusions that end up being disseminated by the popular media (). This is one of the sources of popular beliefs about medical issues.
Another, more important, source are real confounders. And this takes us back to the issue of height being associated with heart disease. In fact, height will typically be significantly associated with heart disease in almost any study that includes men and women and does not control for biological sex.
One of the reasons is that women overall tend to have a significantly lower incident of heart disease than men. The other is that height is significantly lower among women than men, on average, even though there are several women who are taller than the average man.
The table above was from a study including both sexes. Therefore, the strong association between height and arterial stiffness is a “reflection” of the strong association between being male and increased arterial stiffness. If one were to add a variable coded as 0 for male and 1 for female, and use it in a multivariate analysis of predictor of arterial stiffness, together with height, the effect of height would probably “disappear”.
Biological sex is the control variable, the “confounder”, that the authors should have used to narrow down the “true” causes of arterial stiffness (second column in the table). In the absence of biological sex, controlling for height accomplished something similar, but in a “wobbly” way, leaving many readers scratching their heads in confusion.
Take a look at the table below, which I blogged about in a previous post (). This table shows that there is a strong unadjusted correlation between height and arterial stiffness, a marker of heart disease. The likelihood that the correlation is due to chance is lower than one tenth of a percentage point (P<.001).
Interestingly, the authors of the study even use height as a control variable to narrow down the “true” causes of arterial stiffness (column with adjusted results), assuming that height did indeed influence arterial stiffness and what they found to be a key predictor of arterial stiffness, 2-hour postprandial glucose.
But there is no convincing evidence that height causes heart disease, with exception of pathological extremes – e.g., acromegaly. Extremes tend to influence statistical results somewhat, leading to conflicting conclusions that end up being disseminated by the popular media (). This is one of the sources of popular beliefs about medical issues.
Another, more important, source are real confounders. And this takes us back to the issue of height being associated with heart disease. In fact, height will typically be significantly associated with heart disease in almost any study that includes men and women and does not control for biological sex.
One of the reasons is that women overall tend to have a significantly lower incident of heart disease than men. The other is that height is significantly lower among women than men, on average, even though there are several women who are taller than the average man.
The table above was from a study including both sexes. Therefore, the strong association between height and arterial stiffness is a “reflection” of the strong association between being male and increased arterial stiffness. If one were to add a variable coded as 0 for male and 1 for female, and use it in a multivariate analysis of predictor of arterial stiffness, together with height, the effect of height would probably “disappear”.
Biological sex is the control variable, the “confounder”, that the authors should have used to narrow down the “true” causes of arterial stiffness (second column in the table). In the absence of biological sex, controlling for height accomplished something similar, but in a “wobbly” way, leaving many readers scratching their heads in confusion.
Monday, November 26, 2012
No fat gain while eating well during the Holiday Season: Palatability isolines, the 14-percent advantage, and nature’s special spice
Like most animals, our Paleolithic ancestors had to regularly undergo short periods of low calorie intake. If they were successful at procuring food, those ancestors alternated between periods of mild famine and feast. As a result, nature allowed them to survive and leave offspring. The periods of feast likely involved higher-than-average consumption of animal foods, with the opposite probably being true in periods of mild famine.
Almost anyone who adopted a low carbohydrate diet for a while will tell you that they find foods previously perceived as bland, such as carrots or walnuts, to taste very sweet – meaning, to taste very good. This is a special case of a more general phenomenon. If a nutrient is important for your body, and your body is deficient in it, those foods that contain the nutrient will taste very good.
This rule of thumb applies primarily to foods that contributed to selection pressures in our evolutionary past. Mostly these were foods available in our Paleolithic evolutionary past, although some populations may have developed divergent partial adaptations to more modern foods due to recent yet acute selection pressure. Because of the complexity of the dietary nutrient absorption process, involving many genes, I suspect that the vast majority of adaptations to modern foods are partial adaptations.
Modern engineered foods are designed to bypass reward mechanisms that match nutrient content with deficiency levels. That is not the case with more natural foods, which tend to taste good only to the extent that the nutrients that they carry are needed by our bodies.
Consequently palatability is not fixed for a particular natural food; it does not depend only on the nutrient content of the food. It also depends on the body’s deficiency with respect to the nutrient that the food contains. Below is what you would get if you were to plot a surface that best fit a set of data points relating palatability of a specific food item, nutrient content of that food, and the level of nutrient deficiency, for a group of people. I generated the data through a simple simulation, with added error to make the simulation more realistic.
Based on this best-fitting surface you could then generate a contour graph, shown below. The curves are “contour lines”, a.k.a. isolines. Each isoline refers to palatability values that are constant for a set of nutrient content and nutrient deficiency combinations. Next to the isolines are the corresponding palatability values, which vary from about 10 to 100. As you can see, palatability generally goes up as one moves toward to right-top corner of the graph, which is the area where nutrient content and nutrient deficiency are both high.
What happens when the body is in short-term nutrient deficiency with respect to a nutrient? One thing that happens is an increase in enzymatic activity, often referred to by the more technical term “phosphorylation”. Enzymes are typically proteins that cause an acute and targeted increase in specific metabolic processes. Many diseases are associated with dysfunctional enzyme activity. Short-term nutrient deficiency causes enzymatic activity associated with absorption and retention of the nutrient to go up significantly. In other words, your body holds on to its reserves of the nutrient, and becomes much more responsive to dietary intake of the nutrient.
The result is predictable, but many people seem to be unaware of it; most are actually surprised by it. If the nutrient in question is a macro-nutrient, it will be allocated in such a way that less of it will go into our calorie stores – namely adipocytes (body fat). This applies even to dietary fat itself, as fat is needed throughout the body for functions other than energy storage. I have heard from many people who, by alternating between short-term fasting and feasting, lost body fat while maintaining the same calorie intake as in a previous period when they were steadily gaining body fat without any fasting. Invariably they were very surprised by what happened.
In a diet of mostly natural foods, with minimal intake of industrialized foods, short-term calorie deficiency is usually associated with short-term deficiency of various nutrients. Short-term calorie deficiency, when followed by significant calorie surplus (i.e., eating little and then a lot), is associated with a phenomenon I blogged about before here – the “14-percent advantage” of eating little and then a lot (, ). Underfeeding and then overfeeding leads to a reduction in the caloric value of the meals during overfeeding; a reduction of about 14 percent of the overfed amount.
So, how can you go through the Holiday Season giving others the impression that you eat as much as you want, and do not gain any body fat (maybe even lose some)? Eat very little, or fast, in those days where there will be a feast (Thanksgiving dinner); and then eat to satisfaction during the feast, staying away from industrialized foods as much as possible. Everything will taste extremely delicious, as nature’s “special spice” is hunger. And you may even lose body fat in the process!
But there is a problem. Our bodies are not designed to associate eating very little, or not at all, with pleasure. Yet another thing that we can blame squarely on evolution! Success takes practice and determination, aided by the expectation of delayed gratification.
Almost anyone who adopted a low carbohydrate diet for a while will tell you that they find foods previously perceived as bland, such as carrots or walnuts, to taste very sweet – meaning, to taste very good. This is a special case of a more general phenomenon. If a nutrient is important for your body, and your body is deficient in it, those foods that contain the nutrient will taste very good.
This rule of thumb applies primarily to foods that contributed to selection pressures in our evolutionary past. Mostly these were foods available in our Paleolithic evolutionary past, although some populations may have developed divergent partial adaptations to more modern foods due to recent yet acute selection pressure. Because of the complexity of the dietary nutrient absorption process, involving many genes, I suspect that the vast majority of adaptations to modern foods are partial adaptations.
Modern engineered foods are designed to bypass reward mechanisms that match nutrient content with deficiency levels. That is not the case with more natural foods, which tend to taste good only to the extent that the nutrients that they carry are needed by our bodies.
Consequently palatability is not fixed for a particular natural food; it does not depend only on the nutrient content of the food. It also depends on the body’s deficiency with respect to the nutrient that the food contains. Below is what you would get if you were to plot a surface that best fit a set of data points relating palatability of a specific food item, nutrient content of that food, and the level of nutrient deficiency, for a group of people. I generated the data through a simple simulation, with added error to make the simulation more realistic.
Based on this best-fitting surface you could then generate a contour graph, shown below. The curves are “contour lines”, a.k.a. isolines. Each isoline refers to palatability values that are constant for a set of nutrient content and nutrient deficiency combinations. Next to the isolines are the corresponding palatability values, which vary from about 10 to 100. As you can see, palatability generally goes up as one moves toward to right-top corner of the graph, which is the area where nutrient content and nutrient deficiency are both high.
What happens when the body is in short-term nutrient deficiency with respect to a nutrient? One thing that happens is an increase in enzymatic activity, often referred to by the more technical term “phosphorylation”. Enzymes are typically proteins that cause an acute and targeted increase in specific metabolic processes. Many diseases are associated with dysfunctional enzyme activity. Short-term nutrient deficiency causes enzymatic activity associated with absorption and retention of the nutrient to go up significantly. In other words, your body holds on to its reserves of the nutrient, and becomes much more responsive to dietary intake of the nutrient.
The result is predictable, but many people seem to be unaware of it; most are actually surprised by it. If the nutrient in question is a macro-nutrient, it will be allocated in such a way that less of it will go into our calorie stores – namely adipocytes (body fat). This applies even to dietary fat itself, as fat is needed throughout the body for functions other than energy storage. I have heard from many people who, by alternating between short-term fasting and feasting, lost body fat while maintaining the same calorie intake as in a previous period when they were steadily gaining body fat without any fasting. Invariably they were very surprised by what happened.
In a diet of mostly natural foods, with minimal intake of industrialized foods, short-term calorie deficiency is usually associated with short-term deficiency of various nutrients. Short-term calorie deficiency, when followed by significant calorie surplus (i.e., eating little and then a lot), is associated with a phenomenon I blogged about before here – the “14-percent advantage” of eating little and then a lot (, ). Underfeeding and then overfeeding leads to a reduction in the caloric value of the meals during overfeeding; a reduction of about 14 percent of the overfed amount.
So, how can you go through the Holiday Season giving others the impression that you eat as much as you want, and do not gain any body fat (maybe even lose some)? Eat very little, or fast, in those days where there will be a feast (Thanksgiving dinner); and then eat to satisfaction during the feast, staying away from industrialized foods as much as possible. Everything will taste extremely delicious, as nature’s “special spice” is hunger. And you may even lose body fat in the process!
But there is a problem. Our bodies are not designed to associate eating very little, or not at all, with pleasure. Yet another thing that we can blame squarely on evolution! Success takes practice and determination, aided by the expectation of delayed gratification.
Monday, November 12, 2012
The bipolar disorder pendulum: Depression as a compensatory adaptation
As far as explaining natural phenomena, Darwin was one of the best theoretical researchers of all time. Yet, there were a few phenomena that puzzled him for many years. One was the evolution of survival-impairing traits such as the peacock’s train, the large and brightly colored tail appendage observed in males.
Tha male peacock’s train is detrimental to the animal’s survival, and yet it is clearly an evolved trait ().
This type of trait is known as a “costly” trait – a trait that enhances biological fitness (or reproductive success, not to be confused with “gym fitness”), and yet is detrimental to the survival of the individuals who possess it (). Many costly traits have evolved in animals because of sexual selection. That is, they have evolved because they are sexy.
Costly traits seem like a contradiction in terms, but the mechanisms by which they can evolve become clear when evolution is modeled mathematically (, ). There is evidence that mental disorders may have evolved as costs of attractive mental traits (); one in particular, bipolar disorder (a.k.a. manic-depression), fits this hypothesis quite well.
Ironically, a key contributor to the mathematics used to understand costly traits, George R. Price (), might have suffered from severe bipolar disorder. Most of Price’s work in evolutionary biology was done in the 1970s; toward the end of his life, which was untimely ended by Price himself. For many years he was known mostly by evolutionary biologists, but this has changed recently with the publication of Oren Harman’s superb biographical book titled “The Price of Altruism: George Price and the Search for the Origins of Kindness” ().
Bipolar disorder is a condition characterized by disruptive mood swings. These swings are between manic and depressed states, and are analogous to the movement of a pendulum in that they alternate, seemingly gravitating around the "normal" state. See the figurative pendulum representation below, adapted from a drawing on Thinkquest.org.
Bipolar disorder is generally associated with creative intelligence, which is a very attractive trait (). Moreover, the manic state of the disorder is associated with hypersexuality and exaggerated generosity (). So one can clearly see how having bipolar disorder may lead to greater reproductive success, even as it creates long-term survival problems.
On one hand, a person may become very energetic and creative while in the manic state. This could be one of the reasons why many who suffer from bipolar disorder have fairly successful careers in fields that require creative intelligence (), which are many and not restricted to fields related to the fine and performing arts. Creative intelligence is highly valued in most knowledge-intensive professions ().
On the other hand, sustained acute mania or depression are frequently associated with serious health problems (). This is why the clinical treatment of bipolar disorder often starts with an attempt to keep the pendulum from moving too far in one direction or another. This may require medication, such as clinical doses of the elemental salt lithium, prior to cognitive behavioral therapy. The focus of cognitive behavioral therapy is on changing the way one sees and thinks about the world, particularly one’s “social world”.
Prolonged acute mania, usually accompanied by severely impaired sleep, may lead to psychosis. This, psychosis, is an extreme state characterized by hallucinations and/or delusions, leading to hospitalization in most cases. It has been theorized that depression is an involuntary compensatory adaptation () aimed at moving the pendulum in the other direction, out of the manic state, before more damage ensues ().
Elaborate approaches have been devised to treat and manage bipolar disorder treatment that involve the identification of mania and depression “prodromes” (), which are signs that a full-blown manic or depressive episode is about to start. Once prodromes are identified, cognitive behavioral therapy techniques are employed to prevent the pendulum from moving further in one direction or the other. The main goal of these techniques is to change one’s way of thinking about various issues (e.g., fears, pessimism). These techniques take years of practice to be used effectively.
Identification of prodromes and subsequent use of cognitive behavioral therapy seems to be particularly effective when dutifully applied with respect to manic episodes (). The reason for this may be related to one interesting fact related to bipolar disorder: manic episodes are not normally dreaded as much as depression episodes.
In fact, many sufferers avoid taking medication because they do not want to give up the creative and energetic bursts that come with manic episodes, even though they absolutely do not want the pendulum to go in the other direction. The problem is that, if depression is indeed a compensatory adaptation to mania, it seems reasonable to assume that extreme manic episodes are likely to be followed by extreme episodes of depression. Perhaps the key to avoid prolonged acute depression is to avoid prolonged acute mania.
As someone with bipolar disorder becomes more and more excited with novel and racing thoughts (a prodrome of mania), it would probably make sense to identify and carry out calming activities – to avoid a fall into despairing depression afterwards.
Tha male peacock’s train is detrimental to the animal’s survival, and yet it is clearly an evolved trait ().
This type of trait is known as a “costly” trait – a trait that enhances biological fitness (or reproductive success, not to be confused with “gym fitness”), and yet is detrimental to the survival of the individuals who possess it (). Many costly traits have evolved in animals because of sexual selection. That is, they have evolved because they are sexy.
Costly traits seem like a contradiction in terms, but the mechanisms by which they can evolve become clear when evolution is modeled mathematically (, ). There is evidence that mental disorders may have evolved as costs of attractive mental traits (); one in particular, bipolar disorder (a.k.a. manic-depression), fits this hypothesis quite well.
Ironically, a key contributor to the mathematics used to understand costly traits, George R. Price (), might have suffered from severe bipolar disorder. Most of Price’s work in evolutionary biology was done in the 1970s; toward the end of his life, which was untimely ended by Price himself. For many years he was known mostly by evolutionary biologists, but this has changed recently with the publication of Oren Harman’s superb biographical book titled “The Price of Altruism: George Price and the Search for the Origins of Kindness” ().
Bipolar disorder is a condition characterized by disruptive mood swings. These swings are between manic and depressed states, and are analogous to the movement of a pendulum in that they alternate, seemingly gravitating around the "normal" state. See the figurative pendulum representation below, adapted from a drawing on Thinkquest.org.
Bipolar disorder is generally associated with creative intelligence, which is a very attractive trait (). Moreover, the manic state of the disorder is associated with hypersexuality and exaggerated generosity (). So one can clearly see how having bipolar disorder may lead to greater reproductive success, even as it creates long-term survival problems.
On one hand, a person may become very energetic and creative while in the manic state. This could be one of the reasons why many who suffer from bipolar disorder have fairly successful careers in fields that require creative intelligence (), which are many and not restricted to fields related to the fine and performing arts. Creative intelligence is highly valued in most knowledge-intensive professions ().
On the other hand, sustained acute mania or depression are frequently associated with serious health problems (). This is why the clinical treatment of bipolar disorder often starts with an attempt to keep the pendulum from moving too far in one direction or another. This may require medication, such as clinical doses of the elemental salt lithium, prior to cognitive behavioral therapy. The focus of cognitive behavioral therapy is on changing the way one sees and thinks about the world, particularly one’s “social world”.
Prolonged acute mania, usually accompanied by severely impaired sleep, may lead to psychosis. This, psychosis, is an extreme state characterized by hallucinations and/or delusions, leading to hospitalization in most cases. It has been theorized that depression is an involuntary compensatory adaptation () aimed at moving the pendulum in the other direction, out of the manic state, before more damage ensues ().
Elaborate approaches have been devised to treat and manage bipolar disorder treatment that involve the identification of mania and depression “prodromes” (), which are signs that a full-blown manic or depressive episode is about to start. Once prodromes are identified, cognitive behavioral therapy techniques are employed to prevent the pendulum from moving further in one direction or the other. The main goal of these techniques is to change one’s way of thinking about various issues (e.g., fears, pessimism). These techniques take years of practice to be used effectively.
Identification of prodromes and subsequent use of cognitive behavioral therapy seems to be particularly effective when dutifully applied with respect to manic episodes (). The reason for this may be related to one interesting fact related to bipolar disorder: manic episodes are not normally dreaded as much as depression episodes.
In fact, many sufferers avoid taking medication because they do not want to give up the creative and energetic bursts that come with manic episodes, even though they absolutely do not want the pendulum to go in the other direction. The problem is that, if depression is indeed a compensatory adaptation to mania, it seems reasonable to assume that extreme manic episodes are likely to be followed by extreme episodes of depression. Perhaps the key to avoid prolonged acute depression is to avoid prolonged acute mania.
As someone with bipolar disorder becomes more and more excited with novel and racing thoughts (a prodrome of mania), it would probably make sense to identify and carry out calming activities – to avoid a fall into despairing depression afterwards.
Monday, October 1, 2012
The anatomy of a VAP test report
The vertical auto profile (VAP) test is an enhanced lipid profile test. It has been proposed, as a more complete test that relies on direct measurement of previously calculated lipid measures. The VAP test is particularly known for providing direct measurements of LDL cholesterol, instead of calculating them through equations ().
At the time of this writing, a typical VAP test report would provide direct measures of the cholesterol content of LDL, Lp(a), IDL, HDL, and VLDL particles. It would also provide additional measures referred to as secondary risk factors, notably particle density patterns and apolipoprotein concentrations. Finally, it would provide a customized risk summary and some basic recommendations for treatment. Below is the top part of a typical VAP test report (from the company Atherotech), showing measures of the cholesterol content of various particles. LDL cholesterol is combined for four particle subtypes, the small-dense subtypes 4 and 3, and the large-buoyant subtypes 2 and 1. A breakdown by LDL particle subtype is provided later in the VAP report.
In the table above, HDL cholesterol is categorized in two subtypes, the small-dense subtype 2, and the large-buoyant subtype 3. Interestingly, most of the HDL cholesterol in the table is supposedly of the least protective subtype, which seems to be a common finding in the general population. VLDL cholesterol is categorized in a similar way. IDL stands for intermediate-density lipoprotein; this is essentially a VLDL particle that has given off some of its content, particularly its triglyceride (or fat) cargo, but still remains in circulation.
Lp(a) is a special subtype of the LDL particle that is purported to be associated with markedly atherogenic factors. Mainstream medicine generally considers Lp(a) particles themselves to be atherogenic, which is highly debatable. Among other things, cardiovascular disease (CVD) risk and Lp(a) concentration follow a J-curve pattern, and Lp(a)’s range of variation in humans is very large. A blog post by Peter (Hyperlipid) has a figure right at the top that illustrates the former J-curve assertion (). The latter fact, related to range of variation, generally leads to a rather wide normal distribution of Lp(a) concentrations in most populations; meaning that a large number of individuals tend to fall outside Lp(a)’s optimal range and still have a low risk of developing CVD.
Below is the middle part of a typical VAP report, showing secondary risk factors, such as particle density patterns and apolipoprotein concentrations. LDL particle pattern A is considered to be the most protective, supposedly because large-buoyant LDL particles are less likely to penetrate the endothelial gaps, which are about 25 nm in diameter. Apolipoproteins are proteins that bind to fats for their transport in lipoproteins, to be used by various tissues for energy; free fatty acids also need to bind to proteins, notably albumin, to be transported to tissues for use as energy. Redundant particles and processes are everywhere in the human body!
Below is the bottom part of a typical VAP report, providing a risk summary and some basic recommendations. One of the recommendations is “to lower” the LDL target from 130mg/dL to 100mg/dL due to the presence of the checked emerging risk factors on the right, under “Considerations”. What that usually means in practice is a recommendation to take drugs, especially statins, to reduce LDL cholesterol levels. A recent post here and the discussion under it suggest that this would be a highly questionable recommendation in the vast majority of cases ().
What do I think about VAP tests? I think that they are useful in that they provide a lot more information about one’s lipids than standard lipid profiles, and more information is better than less. On the other hand, I think that people should be very careful about what they do with that information. There are even more direct tests that I would recommend before a decision to take drugs is made (, ), if that decision is ever made at all.
At the time of this writing, a typical VAP test report would provide direct measures of the cholesterol content of LDL, Lp(a), IDL, HDL, and VLDL particles. It would also provide additional measures referred to as secondary risk factors, notably particle density patterns and apolipoprotein concentrations. Finally, it would provide a customized risk summary and some basic recommendations for treatment. Below is the top part of a typical VAP test report (from the company Atherotech), showing measures of the cholesterol content of various particles. LDL cholesterol is combined for four particle subtypes, the small-dense subtypes 4 and 3, and the large-buoyant subtypes 2 and 1. A breakdown by LDL particle subtype is provided later in the VAP report.
In the table above, HDL cholesterol is categorized in two subtypes, the small-dense subtype 2, and the large-buoyant subtype 3. Interestingly, most of the HDL cholesterol in the table is supposedly of the least protective subtype, which seems to be a common finding in the general population. VLDL cholesterol is categorized in a similar way. IDL stands for intermediate-density lipoprotein; this is essentially a VLDL particle that has given off some of its content, particularly its triglyceride (or fat) cargo, but still remains in circulation.
Lp(a) is a special subtype of the LDL particle that is purported to be associated with markedly atherogenic factors. Mainstream medicine generally considers Lp(a) particles themselves to be atherogenic, which is highly debatable. Among other things, cardiovascular disease (CVD) risk and Lp(a) concentration follow a J-curve pattern, and Lp(a)’s range of variation in humans is very large. A blog post by Peter (Hyperlipid) has a figure right at the top that illustrates the former J-curve assertion (). The latter fact, related to range of variation, generally leads to a rather wide normal distribution of Lp(a) concentrations in most populations; meaning that a large number of individuals tend to fall outside Lp(a)’s optimal range and still have a low risk of developing CVD.
Below is the middle part of a typical VAP report, showing secondary risk factors, such as particle density patterns and apolipoprotein concentrations. LDL particle pattern A is considered to be the most protective, supposedly because large-buoyant LDL particles are less likely to penetrate the endothelial gaps, which are about 25 nm in diameter. Apolipoproteins are proteins that bind to fats for their transport in lipoproteins, to be used by various tissues for energy; free fatty acids also need to bind to proteins, notably albumin, to be transported to tissues for use as energy. Redundant particles and processes are everywhere in the human body!
Below is the bottom part of a typical VAP report, providing a risk summary and some basic recommendations. One of the recommendations is “to lower” the LDL target from 130mg/dL to 100mg/dL due to the presence of the checked emerging risk factors on the right, under “Considerations”. What that usually means in practice is a recommendation to take drugs, especially statins, to reduce LDL cholesterol levels. A recent post here and the discussion under it suggest that this would be a highly questionable recommendation in the vast majority of cases ().
What do I think about VAP tests? I think that they are useful in that they provide a lot more information about one’s lipids than standard lipid profiles, and more information is better than less. On the other hand, I think that people should be very careful about what they do with that information. There are even more direct tests that I would recommend before a decision to take drugs is made (, ), if that decision is ever made at all.
Monday, September 17, 2012
Familial hypercholesteromia: Why rely on cholesterol levels when more direct measures are available?
There are two forms of familial hypercholesteromia (FH), namely heterozygous and homozygous FH. In heterozygous FH only one copy of the gene that causes it is present, inherited either from the father or the mother. In homozygous FH, which is the most lethal form, two copies of the gene are present. FH is associated with early-onset cardiovascular disease (CVD).
Homozygous FH may happen if both the father and mother have heterozygous or homozygous FH. If both the father and mother have heterozygous FH, the likelihood that at least one in four children will have homozygous FH will be high. If both parents have homozygous FH the likelihood that all children will have homozygous FH will be high.
In fact, in the latter case, homozygous FH in the children is almost certain. One case in which it won’t occur is if the combining FH gene from the father or mother mutates into a non-FH gene before it is used in the assembly of the genome of the child. A gene mutation in a specific locus, only for the father or mother, is an unlikely event, and would lead to heterozygous FH. Two gene mutations at once in the same locus, for the father and mother, is a very unlikely event.
By the way, despite what many are led to believe based on fictional characters in movies and series like the X-Men and Hulk, mutations in functional genes usually lead to harmful traits. In our evolutionary past, those traits would have been largely removed from the gene pool by selection, making them rare or nonexistent in modern humans. Today we have modern medicine; a double-edged sword.
Mutations leading to super-human traits are very, very unlikely. The myostatin gene, for example, suppresses muscle growth. And yet the mutations that lead to little or no secretion of the related myostatin protein are very uncommon. Obviously they have not been favored by selection, even though their holders are very muscular – e.g., Germany’s “Incredible Hulky” ().
Okay, back to FH. Xanthelasmas are relatively common among those who suffer from FH (see photo below, from Globalskinatlas.com). They are skin deposits of cholesterol, have a genetic basis, and are NOT always associated with FH. This is important – several people have xanthelasmas but not FH.
FH is a fairly rare disease, even in its heterozygous form, with an overall incidence of approximately 0.2 percent. That is, about 1 in 500 people in the general population will have it. Genetically related groups will see a much higher or lower rate of incidence, as the disease is strongly influenced by a genetic mutation. This genetic mutation is apparently in the LDL receptor gene, located on the short arm of chromosome 19.
The table below, from a study by Miltiadous and colleagues (), paints a broad picture of the differences one would typically see between heterozygous FH sufferers and non-FH controls.
The main difference is in total cholesterol and in the relatively large contribution of LDL to total cholesterol. A large difference is also seen in Apolipoprotein B (indicated as "Apo B"), which acts as a LDL transporter (not to be confused with a LDL receptor). The LDL cholesterol shown on the table is calculated through the Friedewald equation, which is notoriously imprecise at low triglyceride levels ().
Looking at the total cholesterol row on the table, and assuming that the numbers after the plus/minus signs are standard deviations, we can conclude that: (a) a little more than two-thirds of the heterozygous FH sufferers had total cholesterol levels falling in between 280 and 446; and (b) a little more than two-thirds of the non-FH controls had total cholesterol levels falling in between 135 and 225.
Keep in mind that about 13.5 percent {calculated as: (95-68)/2} of the non-FH controls had total cholesterol levels between 225 and 270. This is a nontrivial percentage; i.e., these may be a minority but are not rare individuals. Heterozygous FH sufferers are rare, at 0.2 percent of the general population. Moreover, about 2 percent of the non-FH controls had non-pathological total cholesterol levels between 270 and 315. That is not so rare either, amounting to an “incidence” 10 times higher than heterozygous FH.
What would happen if people with heterozygous FH were to replace refined carbohydrates and sugars with saturated fat and cholesterol in their diets? Very likely their already high total cholesterol would go up higher, in part because their HDL cholesterol would go up (). Still, how could they be sure that CVD progression would accelerate if they did that?
According to some studies, the higher HDL cholesterol would either be generally protective or associated with protective factors, even among those with FH (). One of those protective factors may be a more nutrient-dense diet, as many foods rich in cholesterol are very nutrient-dense – e.g., eggs, organ meats, and seafood.
This brings me to my main point in this post. It is mainstream practice to diagnose people with FH based on total and/or LDL cholesterol levels. But the main problem with FH is that it leads to early onset of CVD, which can be measured more directly through simple tests, such as intima-media thickness and related ultrasound plaque tests (). These are noninvasive tests, done in 5 minutes or so, and often covered by insurance.
Even if simple direct tests are not perfect, it seems utterly nonsensical to rely on cholesterol measures to diagnose and treat FH, given the possible overlap between pathological and non-pathological high total cholesterol levels.
Homozygous FH may happen if both the father and mother have heterozygous or homozygous FH. If both the father and mother have heterozygous FH, the likelihood that at least one in four children will have homozygous FH will be high. If both parents have homozygous FH the likelihood that all children will have homozygous FH will be high.
In fact, in the latter case, homozygous FH in the children is almost certain. One case in which it won’t occur is if the combining FH gene from the father or mother mutates into a non-FH gene before it is used in the assembly of the genome of the child. A gene mutation in a specific locus, only for the father or mother, is an unlikely event, and would lead to heterozygous FH. Two gene mutations at once in the same locus, for the father and mother, is a very unlikely event.
By the way, despite what many are led to believe based on fictional characters in movies and series like the X-Men and Hulk, mutations in functional genes usually lead to harmful traits. In our evolutionary past, those traits would have been largely removed from the gene pool by selection, making them rare or nonexistent in modern humans. Today we have modern medicine; a double-edged sword.
Mutations leading to super-human traits are very, very unlikely. The myostatin gene, for example, suppresses muscle growth. And yet the mutations that lead to little or no secretion of the related myostatin protein are very uncommon. Obviously they have not been favored by selection, even though their holders are very muscular – e.g., Germany’s “Incredible Hulky” ().
Okay, back to FH. Xanthelasmas are relatively common among those who suffer from FH (see photo below, from Globalskinatlas.com). They are skin deposits of cholesterol, have a genetic basis, and are NOT always associated with FH. This is important – several people have xanthelasmas but not FH.
FH is a fairly rare disease, even in its heterozygous form, with an overall incidence of approximately 0.2 percent. That is, about 1 in 500 people in the general population will have it. Genetically related groups will see a much higher or lower rate of incidence, as the disease is strongly influenced by a genetic mutation. This genetic mutation is apparently in the LDL receptor gene, located on the short arm of chromosome 19.
The table below, from a study by Miltiadous and colleagues (), paints a broad picture of the differences one would typically see between heterozygous FH sufferers and non-FH controls.
The main difference is in total cholesterol and in the relatively large contribution of LDL to total cholesterol. A large difference is also seen in Apolipoprotein B (indicated as "Apo B"), which acts as a LDL transporter (not to be confused with a LDL receptor). The LDL cholesterol shown on the table is calculated through the Friedewald equation, which is notoriously imprecise at low triglyceride levels ().
Looking at the total cholesterol row on the table, and assuming that the numbers after the plus/minus signs are standard deviations, we can conclude that: (a) a little more than two-thirds of the heterozygous FH sufferers had total cholesterol levels falling in between 280 and 446; and (b) a little more than two-thirds of the non-FH controls had total cholesterol levels falling in between 135 and 225.
Keep in mind that about 13.5 percent {calculated as: (95-68)/2} of the non-FH controls had total cholesterol levels between 225 and 270. This is a nontrivial percentage; i.e., these may be a minority but are not rare individuals. Heterozygous FH sufferers are rare, at 0.2 percent of the general population. Moreover, about 2 percent of the non-FH controls had non-pathological total cholesterol levels between 270 and 315. That is not so rare either, amounting to an “incidence” 10 times higher than heterozygous FH.
What would happen if people with heterozygous FH were to replace refined carbohydrates and sugars with saturated fat and cholesterol in their diets? Very likely their already high total cholesterol would go up higher, in part because their HDL cholesterol would go up (). Still, how could they be sure that CVD progression would accelerate if they did that?
According to some studies, the higher HDL cholesterol would either be generally protective or associated with protective factors, even among those with FH (). One of those protective factors may be a more nutrient-dense diet, as many foods rich in cholesterol are very nutrient-dense – e.g., eggs, organ meats, and seafood.
This brings me to my main point in this post. It is mainstream practice to diagnose people with FH based on total and/or LDL cholesterol levels. But the main problem with FH is that it leads to early onset of CVD, which can be measured more directly through simple tests, such as intima-media thickness and related ultrasound plaque tests (). These are noninvasive tests, done in 5 minutes or so, and often covered by insurance.
Even if simple direct tests are not perfect, it seems utterly nonsensical to rely on cholesterol measures to diagnose and treat FH, given the possible overlap between pathological and non-pathological high total cholesterol levels.
Monday, September 3, 2012
Daniel Suelo, the man who quit money, seems remarkably healthy
Daniel James Shellabarger (better known as Daniel Suelo) is portrayed in the bestselling 2012 nonfiction book by Mark Sundeen titled “The Man Who Quit Money” ().
Apparently Suelo stopped using money in 2000, and lives in a cave near the city of Moab in Utah. His diet comprises primarily wild vegetables and fruits, insects, and road kill; as well as discarded or donated food he gets from others when he visits the city. The photo below is from a recent BBC documentary. An interesting 2006 YouTube clip on Suelo is titled “Moneyless in Moab” ().
Suelo is listed as having been born in 1961 (), and the photo above appears to have been taken in 2012. If these dates are correct, he is 51 in the photo above. I cannot help but think that he looks remarkably healthy. The 40-50 age period is one that often sets the stage for many diseases of civilization in urban societies.
Suelo’s decision seems like a radical one, at least to me. There are always complex motivations behind radical decisions. In the case of Suelo, some of these motivations are captured in the comment below, which is part of a review of the book “The Man Who Quit Money” posted on Amazon.com by a reader.
Many people have been inspired by Suelo’s story, to some extent because they see that adopting a radical form of “simple living” () may not only be possible but also liberating. Obviously Suelo’s lifestyle, as it is now, would not be possible without the help of others who adopt a more “traditional” lifestyle. Below is a critical review by a reader of the book, posted on Amazon.com, which harshly reflects this perspective.
Still, Suelo’s story is interesting, including from a human health perspective. An article on Details.com by Christopher Ketcham provides a glimpse at what a day in Suelo’s life looks like (). It seems that on most days he has one main meal per day.
It is hard to get a sense of the nutrient composition of his diet. It looks like his diet is limited in but not devoid of industrial foods, and one in which food consumption is sporadic, opportunistic, and driven primarily by hunger and availability – not by stress or set meal times, for example.
He probably walks a lot; his cave is one hour away from Moab by foot, and it looks like he goes to Moab often. Apparently he almost never gets sick.
Suelo also writes a blog (), which has many followers, and also maintains other websites, from the Public Library in Moab. His first blog post has over 1,000 comments under it ().
Apparently Suelo stopped using money in 2000, and lives in a cave near the city of Moab in Utah. His diet comprises primarily wild vegetables and fruits, insects, and road kill; as well as discarded or donated food he gets from others when he visits the city. The photo below is from a recent BBC documentary. An interesting 2006 YouTube clip on Suelo is titled “Moneyless in Moab” ().
Suelo is listed as having been born in 1961 (), and the photo above appears to have been taken in 2012. If these dates are correct, he is 51 in the photo above. I cannot help but think that he looks remarkably healthy. The 40-50 age period is one that often sets the stage for many diseases of civilization in urban societies.
Suelo’s decision seems like a radical one, at least to me. There are always complex motivations behind radical decisions. In the case of Suelo, some of these motivations are captured in the comment below, which is part of a review of the book “The Man Who Quit Money” posted on Amazon.com by a reader.
[…] a picture of Suelo not as an untarnished hero, but a man who has wrestled with heartbreak, depression, disillusionment with his family's faith, and his repugnance to working for the pure sake of making money and buying things. Whether or not you are inspired to follow Suelo's example, this book will make you think.
Many people have been inspired by Suelo’s story, to some extent because they see that adopting a radical form of “simple living” () may not only be possible but also liberating. Obviously Suelo’s lifestyle, as it is now, would not be possible without the help of others who adopt a more “traditional” lifestyle. Below is a critical review by a reader of the book, posted on Amazon.com, which harshly reflects this perspective.
Any infantile mentality charmed by this inane story should simply generalize the message - visualize a world in which all of us live like the parasitic protagonist. How fortunate for Suelo that there are still people who engage in productive work and indirectly and unknowingly keep the human sponge alive […] Suelo never quit money he simply quit contributing anything and continues to survive simply as a parasite.
Still, Suelo’s story is interesting, including from a human health perspective. An article on Details.com by Christopher Ketcham provides a glimpse at what a day in Suelo’s life looks like (). It seems that on most days he has one main meal per day.
It is hard to get a sense of the nutrient composition of his diet. It looks like his diet is limited in but not devoid of industrial foods, and one in which food consumption is sporadic, opportunistic, and driven primarily by hunger and availability – not by stress or set meal times, for example.
He probably walks a lot; his cave is one hour away from Moab by foot, and it looks like he goes to Moab often. Apparently he almost never gets sick.
Suelo also writes a blog (), which has many followers, and also maintains other websites, from the Public Library in Moab. His first blog post has over 1,000 comments under it ().
Monday, August 20, 2012
The 2012 Atherosclerosis egg study: Plaque decreased as LDL increased with consumption of 2.3 eggs per week or more
A new study by David Spence and colleagues, published online in July 2012 in the journal Atherosclerosis (), has been gaining increasing media attention (e.g., ). The article is titled: “Egg yolk consumption and carotid plaque”. As the title implies, the study focuses on egg yolk consumption and its association with carotid artery plaque buildup.
The study argues that “regular consumption of egg yolk should be avoided by persons at risk of cardiovascular disease”. It hints at egg yolks being unhealthy in general, possibly even more so than cigarettes. Solid critiques have already been posted on blogs by Mark Sisson, Chris Masterjohn, and Zoe Harcombe (, , ), among others.
These critiques present valid arguments for why the key findings of the study cannot be accepted, especially the finding that eggs are more dangerous to one’s health than cigarettes. This post is a bit different. It uses the data reported in the study to show that it (the data) suggests that egg consumption is actually health-promoting.
I used the numbers in Table 2 of the article to conduct a test that is rarely if ever conducted in health studies – a moderating effect test. I left out the “egg-yolk years” variable used by the authors, and focused on weekly egg consumption (see Chris’s critique). My analysis, using WarpPLS (), had to be done only visually, because using values from Table 2 meant that I had access only to data on a few variables organized in quintiles. That is, my analysis here using aggregate data is an N=5 analysis; a small sample indeed. The full-text article is not available publicly; Zoe was kind enough to include the data from Table 2 in her critique post.
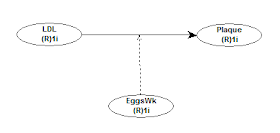
Below is the model that I used for the moderating effect test. It allowed me to look into the effect that the variable EggsWk (number of eggs consumed per week) had on the association between LDL (LDL cholesterol) and Plaque (carotid plaque). This type of effect, namely a moderating effect, is confusing to many people, because it is essentially the effect that a variable has on the effect of another variable on a third. Still, being confusing does not mean being less important. I should note that this type of effect is similar to a type of conditional association tested via Bayesian statistics – if one eats more eggs, what is the association between having a high LDL cholesterol and plaque buildup?
You can see what is happening visually on the graph below. The plot on the left side is for low weekly egg consumption. In it, the association between LDL cholesterol and plaque is positive – eating fewer eggs, plaque and LDL increase together. The plot on the right side is for high weekly egg consumption. In this second plot, the association between LDL cholesterol and plaque is negative – eating more eggs, plaque decreases as LDL increases. And what is the turning point? It is about 2.3 eggs per week.
So the “evil” particle, the LDL, is playing tricks with us; but thankfully the wonderful eggs come to the rescue, right? Well, it looks a bit like it, but maybe other foods would have a similar effect. In part because of the moderating effect discussed above, the multivariate association between LDL cholesterol and plaque was overall negative. This multivariate association was estimated controlling for the moderating effect of weekly egg consumption. You can see this on the plot below.
The highest amount of plaque is at the far left of the plot. It is associated with the lowest LDL cholesterol quintile. (So much for eggs causing plaque via LDL cholesterol eh!?) What is happening here? Maybe egg consumption above a certain level shifts the size of the LDL particles from small to large, making the potentially atherogenic ones harmless. (Saturated fat consumption, in the context of a nutritious diet in lean individuals, seems to have a similar effect.) Maybe eggs contain nutrients that promote overall health, leading LDL particles to "behave" and do what they are supposed to do. Maybe it is a combination of these and other effects.
The study argues that “regular consumption of egg yolk should be avoided by persons at risk of cardiovascular disease”. It hints at egg yolks being unhealthy in general, possibly even more so than cigarettes. Solid critiques have already been posted on blogs by Mark Sisson, Chris Masterjohn, and Zoe Harcombe (, , ), among others.
These critiques present valid arguments for why the key findings of the study cannot be accepted, especially the finding that eggs are more dangerous to one’s health than cigarettes. This post is a bit different. It uses the data reported in the study to show that it (the data) suggests that egg consumption is actually health-promoting.
I used the numbers in Table 2 of the article to conduct a test that is rarely if ever conducted in health studies – a moderating effect test. I left out the “egg-yolk years” variable used by the authors, and focused on weekly egg consumption (see Chris’s critique). My analysis, using WarpPLS (), had to be done only visually, because using values from Table 2 meant that I had access only to data on a few variables organized in quintiles. That is, my analysis here using aggregate data is an N=5 analysis; a small sample indeed. The full-text article is not available publicly; Zoe was kind enough to include the data from Table 2 in her critique post.
Below is the model that I used for the moderating effect test. It allowed me to look into the effect that the variable EggsWk (number of eggs consumed per week) had on the association between LDL (LDL cholesterol) and Plaque (carotid plaque). This type of effect, namely a moderating effect, is confusing to many people, because it is essentially the effect that a variable has on the effect of another variable on a third. Still, being confusing does not mean being less important. I should note that this type of effect is similar to a type of conditional association tested via Bayesian statistics – if one eats more eggs, what is the association between having a high LDL cholesterol and plaque buildup?
You can see what is happening visually on the graph below. The plot on the left side is for low weekly egg consumption. In it, the association between LDL cholesterol and plaque is positive – eating fewer eggs, plaque and LDL increase together. The plot on the right side is for high weekly egg consumption. In this second plot, the association between LDL cholesterol and plaque is negative – eating more eggs, plaque decreases as LDL increases. And what is the turning point? It is about 2.3 eggs per week.
So the “evil” particle, the LDL, is playing tricks with us; but thankfully the wonderful eggs come to the rescue, right? Well, it looks a bit like it, but maybe other foods would have a similar effect. In part because of the moderating effect discussed above, the multivariate association between LDL cholesterol and plaque was overall negative. This multivariate association was estimated controlling for the moderating effect of weekly egg consumption. You can see this on the plot below.
The highest amount of plaque is at the far left of the plot. It is associated with the lowest LDL cholesterol quintile. (So much for eggs causing plaque via LDL cholesterol eh!?) What is happening here? Maybe egg consumption above a certain level shifts the size of the LDL particles from small to large, making the potentially atherogenic ones harmless. (Saturated fat consumption, in the context of a nutritious diet in lean individuals, seems to have a similar effect.) Maybe eggs contain nutrients that promote overall health, leading LDL particles to "behave" and do what they are supposed to do. Maybe it is a combination of these and other effects.
Tuesday, August 14, 2012
Ancestral Health Symposium 2012: Evolutionarily sound diets and lifestyles may revolutionize health care
The Ancestral Health Symposium 2012 was very interesting on many levels. Aaron Blaisdell and the team of volunteers really did a superb job at organizing the Symposium. Boston is a great city with an excellent public transportation system, something that is always great for meetings, and a great choice for the Symposium. Needless to say, so was Harvard. Even though the program was packed there were plenty of opportunities to meet and talk with several people during the breaks.
We had our panel “New Technologies and New Opportunities”, which Paul Jaminet moderated. The panelists were Chris Keller, Chris Kresser, Dan Pardi, and myself. The first photo below, by Bobby Gill, shows Chris Keller speaking; I am on the far left looking at the screen. The second photo, by Beth Mazur, shows all the panelists. The third photo, also by Bobby Gill, shows a group of us talking to Stephan Guyenet after his presentation.
I talked a bit toward the end of the panel about the importance of taking nonlinearity into consideration in analyses of health data, but ended up being remembered later for saying that “men are women with a few design flaws”. I said that to highlight the strong protective effect of being female in terms of health, which was clear from the model I was discussing.
There is a good evolutionary reason for the protective effect of being female. Evolution is a population phenomenon. Genes do not evolve; neither do individuals. Populations evolve through the spread or disappearance of genotypes. A healthy population with 99 men and 1 woman will probably disappear quickly, and so will its gene pool. A healthy population with 99 women and 1 man will probably thrive, even with the drag of inbreeding depression. Under harsh environmental conditions, the rate of female-to-male births goes up, in some cases quite a lot.
I was able to talk to, or at least meet briefly face-to-face with, many of the people that I have interacted with online on this blog and other blogs. Just to name a few: Miki Ben-Dor, Aaron Blaisdell, Emily Deans, Andreas Eenfeldt, Glenn Ellmers, Benjamin Gebhard, Stephan Guyenet, Dallas Hartwig, Melissa Hartwig, Paul Jaminet, Chris Keller, Chris Kresser, Mathieu Lalonde, Robert Lustig, Chris Masterjohn, Beth Mazur, Denise Minger, Jimmy Moore, Katherine Morrison, Richard Nikoley, Dan Pardi, Kamal Patel, David Pendergrass, Mark Sisson, Mary Beth Smrtic, J. Stanton, Carlos Andres Toro, and Grayson Wheatley.
It would have been nice to have Peter (from Hyperlipid) there, as I think a lot of the attendants are fans. I attended Jamie Scott’s very interesting talk, but ended up not being able to chat with him. This is a pity because we share some common experiences – e.g., I lived in New Zealand for a few years. I did have the opportunity to talk at some length with J. Stanton, who is an inspiration. It was also great to exchange some ideas with my panelists, Miki Ben-Dor, Emily Deans, Stephan Guyenet, Chris Masterjohn, Kamal Patel, and David Pendergrass. I wish I had more time to talk with Denise Minger, who is clearly a very nice person in addition to being very smart. Talking about a smart person, it was also nice chatting a bit with Richard Nikoley; a successful entrepreneur who is in the enviable position of doing what he feels like doing.
I could not help but notice a tendency among some participants (perhaps many, judging from online threads) to pay a lot of attention to how other people looked in a very judgmental way. That person is too fat, his/her face is too red, she/he looks too old etc. So was this supposed to be the Ancestral Health Pageant 2012? There is nothing wrong with looking good. But many people adopt an evolution-inspired lifestyle because they are quite unhealthy to start with. And this includes some of the presenters. It takes time to change one’s health, relapses occur, and no one is getting younger. Moreover, some of the presenters’ ideas and advice may have much more dramatic positive effects on people other than themselves, because of their own pre-existing conditions. The ideas and advice are still solid.
A message that I think this Symposium conveyed particularly well was that an evolutionarily sound diet and lifestyle can truly revolutionize our health care system. Robb Wolf’s talk in particular, based on his recent experience in Nevada with law enforcement officers, made this point very effectively. The title of the talk is “How Markets and Evolution Can Revolutionize Medicine”. One very interesting idea he put forth was that establishments like gyms could expand the range of support activities they offer their customers, officially becoming the beginning of the health care chain. There are already health insurance plans that offer premium reductions for those who go to gyms. Being part of the health care chain would be different and a significant step forward - diet and exercise are powerful "drugs".
One thing that caught me a bit off-guard was Robb’s strong advocacy of the use of a drug, namely metformin (a.k.a. glucophage); even preventively in some special cases, such as with sleep-deprived law enforcement officers. I have to listen to that talk again when it is up online, to make sure that I understood it correctly. It seems to me that changing the nature of shift work among law enforcement officers, at least partially, may be a better target; current practices appear not only to impair the officers’ health but also their effectiveness in law enforcement activities. Besides, I think we need to better understand the nature and functions of cortisol, which is viewed by many as a hormone that exists only to do us harm.
Sleep deprivation is associated with an elevation in cortisol production. Elevated cortisol levels lead over time to visceral fat accumulation, which promotes systemic inflammation. Systemic inflammation is possibly the root cause of most diseases of civilization. But cortisol itself has powerful anti-inflammatory properties, and visceral fat is generally easy to mobilize through intense exercise – probably one of the key reasons why we have visceral fat. I think we need to understand this situation a bit better before thinking about preventive uses of metformin, which nevertheless is a drug that seems to do wonders in the treatment of type 2 diabetes.
Beth Mazur was kind enough to put up a post with links to various Ancestral Health Symposium 2012 summary posts, as well as pictures. Paul Jaminet has a post with an insightful discussion of our panel at the Symposium.
We had our panel “New Technologies and New Opportunities”, which Paul Jaminet moderated. The panelists were Chris Keller, Chris Kresser, Dan Pardi, and myself. The first photo below, by Bobby Gill, shows Chris Keller speaking; I am on the far left looking at the screen. The second photo, by Beth Mazur, shows all the panelists. The third photo, also by Bobby Gill, shows a group of us talking to Stephan Guyenet after his presentation.
I talked a bit toward the end of the panel about the importance of taking nonlinearity into consideration in analyses of health data, but ended up being remembered later for saying that “men are women with a few design flaws”. I said that to highlight the strong protective effect of being female in terms of health, which was clear from the model I was discussing.
There is a good evolutionary reason for the protective effect of being female. Evolution is a population phenomenon. Genes do not evolve; neither do individuals. Populations evolve through the spread or disappearance of genotypes. A healthy population with 99 men and 1 woman will probably disappear quickly, and so will its gene pool. A healthy population with 99 women and 1 man will probably thrive, even with the drag of inbreeding depression. Under harsh environmental conditions, the rate of female-to-male births goes up, in some cases quite a lot.
I was able to talk to, or at least meet briefly face-to-face with, many of the people that I have interacted with online on this blog and other blogs. Just to name a few: Miki Ben-Dor, Aaron Blaisdell, Emily Deans, Andreas Eenfeldt, Glenn Ellmers, Benjamin Gebhard, Stephan Guyenet, Dallas Hartwig, Melissa Hartwig, Paul Jaminet, Chris Keller, Chris Kresser, Mathieu Lalonde, Robert Lustig, Chris Masterjohn, Beth Mazur, Denise Minger, Jimmy Moore, Katherine Morrison, Richard Nikoley, Dan Pardi, Kamal Patel, David Pendergrass, Mark Sisson, Mary Beth Smrtic, J. Stanton, Carlos Andres Toro, and Grayson Wheatley.
It would have been nice to have Peter (from Hyperlipid) there, as I think a lot of the attendants are fans. I attended Jamie Scott’s very interesting talk, but ended up not being able to chat with him. This is a pity because we share some common experiences – e.g., I lived in New Zealand for a few years. I did have the opportunity to talk at some length with J. Stanton, who is an inspiration. It was also great to exchange some ideas with my panelists, Miki Ben-Dor, Emily Deans, Stephan Guyenet, Chris Masterjohn, Kamal Patel, and David Pendergrass. I wish I had more time to talk with Denise Minger, who is clearly a very nice person in addition to being very smart. Talking about a smart person, it was also nice chatting a bit with Richard Nikoley; a successful entrepreneur who is in the enviable position of doing what he feels like doing.
I could not help but notice a tendency among some participants (perhaps many, judging from online threads) to pay a lot of attention to how other people looked in a very judgmental way. That person is too fat, his/her face is too red, she/he looks too old etc. So was this supposed to be the Ancestral Health Pageant 2012? There is nothing wrong with looking good. But many people adopt an evolution-inspired lifestyle because they are quite unhealthy to start with. And this includes some of the presenters. It takes time to change one’s health, relapses occur, and no one is getting younger. Moreover, some of the presenters’ ideas and advice may have much more dramatic positive effects on people other than themselves, because of their own pre-existing conditions. The ideas and advice are still solid.
A message that I think this Symposium conveyed particularly well was that an evolutionarily sound diet and lifestyle can truly revolutionize our health care system. Robb Wolf’s talk in particular, based on his recent experience in Nevada with law enforcement officers, made this point very effectively. The title of the talk is “How Markets and Evolution Can Revolutionize Medicine”. One very interesting idea he put forth was that establishments like gyms could expand the range of support activities they offer their customers, officially becoming the beginning of the health care chain. There are already health insurance plans that offer premium reductions for those who go to gyms. Being part of the health care chain would be different and a significant step forward - diet and exercise are powerful "drugs".
One thing that caught me a bit off-guard was Robb’s strong advocacy of the use of a drug, namely metformin (a.k.a. glucophage); even preventively in some special cases, such as with sleep-deprived law enforcement officers. I have to listen to that talk again when it is up online, to make sure that I understood it correctly. It seems to me that changing the nature of shift work among law enforcement officers, at least partially, may be a better target; current practices appear not only to impair the officers’ health but also their effectiveness in law enforcement activities. Besides, I think we need to better understand the nature and functions of cortisol, which is viewed by many as a hormone that exists only to do us harm.
Sleep deprivation is associated with an elevation in cortisol production. Elevated cortisol levels lead over time to visceral fat accumulation, which promotes systemic inflammation. Systemic inflammation is possibly the root cause of most diseases of civilization. But cortisol itself has powerful anti-inflammatory properties, and visceral fat is generally easy to mobilize through intense exercise – probably one of the key reasons why we have visceral fat. I think we need to understand this situation a bit better before thinking about preventive uses of metformin, which nevertheless is a drug that seems to do wonders in the treatment of type 2 diabetes.
Beth Mazur was kind enough to put up a post with links to various Ancestral Health Symposium 2012 summary posts, as well as pictures. Paul Jaminet has a post with an insightful discussion of our panel at the Symposium.
Tuesday, July 31, 2012
The 14-percent advantage of eating little and then a lot: Putting it in practice
In another post () I discussed evidence that the human body may react to “eating big” as it would to overfeeding, increasing energy expenditure by a certain amount. That increase seems to lead to a reduction in the caloric value of the meals during overfeeding; a reduction that seems to gravitate around 14 percent of the overfed amount.
And what is the overfed amount? Let us assume that your daily calorie intake to maintain your current body weight is 2,000 calories. However, one day you consume 1,000 calories, and the next 3,000 – adding up to 4,000 calories in 2 days. This amounts to 2,000 calories per day on average, the weight maintenance amount; but the extra 1,000 on the second day is perceived by your body as overfeeding. So 140 calories are “lost”.
The mechanisms by which this could happen are not entirely clear. Some studies contain clues; one example is the 2002 study conducted with mice by Anson and colleagues (), from which the graphs below were taken.
In the graphs above AL refers to ad libitum feeding, LDF to limited daily feeding (40 percent less than AL), IF to intermittent (alternate-day) fasting, and PF to pair-fed mice that were provided daily with a food allotment equal to the average daily intake of mice in the IF group. PF was added as a control condition; in practice, the 2-day food consumption was about the same in AL, IF and PF.
After a 20-week period, intermittent fasting was associated with the lowest blood glucose and insulin concentrations (graphs a and b), and the highest concentrations of insulin growth factor 1 and ketones (graphs c and d). These seem to be fairly positive outcomes. In humans, they would normally be associated with metabolic improvements and body fat loss.
Let us go back to the 14 percent advantage of eating little and then a lot; a pattern of eating that can be implemented though intermittent fasting, as well as other approaches.
So it seems that if you consume the same number of calories, but you do that while alternating between underfeeding and overfeeding, you actually “absorb” 14 percent fewer calories – with that percentage applied to the extra calorie intake above the amount needed for weight maintenance.
And here is a critical point: energy expenditure does not seem to be significantly reduced by underfeeding, as long as it is short-term underfeeding – e.g., about 24 h or less. So you don’t “gain back” the calories due to a possible reduction in energy expenditure in the (relatively short) underfeeding period.
What do 140 calories mean in terms of fat loss? Just divide that amount by 9 to get an estimate; about 15 g of fat lost. This is about 1 lb per month, and 12 lbs per year. Does one lose muscle due to this, in addition to body fat? A period of underfeeding of about 24 h or less should not be enough to lead to loss of muscle, as long as one doesn’t do glycogen-depleting exercise during that period ().
Also, underfeeding appears to increase the body’s receptivity to both micronutrients and macronutrients. This applies to protein, carbohydrates, vitamins etc. For example, the activity of liver and muscle glycogen synthase is significantly increased by underfeeding (the scientific term is “phosphorylation”), particularly carbohydrate underfeeding, effectively raising the insulin sensitivity of those tissues.
The same happens, in general terms, with a host of other tissues and nutrients; often mediated by enzymes. This means that after a short period of underfeeding your body is primed to absorb micronutrients and macronutrients more effectively, even as it uses up some extra calories – leading to a 14 percent increase in energy expenditure.
There are many ways in which this can be achieved. Intermittent fasting is one of them; with 16-h to 24-h fasts, for example. Intermittent calorie restriction is another; e.g., with a 1/3 and 2/3 calorie consumption pattern across two-day periods. Yet another is intermittent carbohydrate restriction, with other macronutrients kept more or less constant.
If the same amount of food is consumed, there is evidence suggesting that such practices would lead to body weight preservation with improved body composition – same body weight, but reduced fat mass. This is what the study by Anson and colleagues, mentioned earlier, suggested.
A 2005 study by Heilbronn and colleagues on alternate day fasting by humans suggested a small decrease in body weight (); although the loss was clearly mostly of fat mass. Interestingly, this study with nonobese humans suggested a massive decrease in fasting insulin, much like the mice study by Anson and colleagues.
Having said all of the above, there may be people who gain body fat by alternating between eating little and a lot. Why would that be? A possible reason is that when they eat a lot their caloric intake exceeds the increased energy expenditure.
And what is the overfed amount? Let us assume that your daily calorie intake to maintain your current body weight is 2,000 calories. However, one day you consume 1,000 calories, and the next 3,000 – adding up to 4,000 calories in 2 days. This amounts to 2,000 calories per day on average, the weight maintenance amount; but the extra 1,000 on the second day is perceived by your body as overfeeding. So 140 calories are “lost”.
The mechanisms by which this could happen are not entirely clear. Some studies contain clues; one example is the 2002 study conducted with mice by Anson and colleagues (), from which the graphs below were taken.
In the graphs above AL refers to ad libitum feeding, LDF to limited daily feeding (40 percent less than AL), IF to intermittent (alternate-day) fasting, and PF to pair-fed mice that were provided daily with a food allotment equal to the average daily intake of mice in the IF group. PF was added as a control condition; in practice, the 2-day food consumption was about the same in AL, IF and PF.
After a 20-week period, intermittent fasting was associated with the lowest blood glucose and insulin concentrations (graphs a and b), and the highest concentrations of insulin growth factor 1 and ketones (graphs c and d). These seem to be fairly positive outcomes. In humans, they would normally be associated with metabolic improvements and body fat loss.
Let us go back to the 14 percent advantage of eating little and then a lot; a pattern of eating that can be implemented though intermittent fasting, as well as other approaches.
So it seems that if you consume the same number of calories, but you do that while alternating between underfeeding and overfeeding, you actually “absorb” 14 percent fewer calories – with that percentage applied to the extra calorie intake above the amount needed for weight maintenance.
And here is a critical point: energy expenditure does not seem to be significantly reduced by underfeeding, as long as it is short-term underfeeding – e.g., about 24 h or less. So you don’t “gain back” the calories due to a possible reduction in energy expenditure in the (relatively short) underfeeding period.
What do 140 calories mean in terms of fat loss? Just divide that amount by 9 to get an estimate; about 15 g of fat lost. This is about 1 lb per month, and 12 lbs per year. Does one lose muscle due to this, in addition to body fat? A period of underfeeding of about 24 h or less should not be enough to lead to loss of muscle, as long as one doesn’t do glycogen-depleting exercise during that period ().
Also, underfeeding appears to increase the body’s receptivity to both micronutrients and macronutrients. This applies to protein, carbohydrates, vitamins etc. For example, the activity of liver and muscle glycogen synthase is significantly increased by underfeeding (the scientific term is “phosphorylation”), particularly carbohydrate underfeeding, effectively raising the insulin sensitivity of those tissues.
The same happens, in general terms, with a host of other tissues and nutrients; often mediated by enzymes. This means that after a short period of underfeeding your body is primed to absorb micronutrients and macronutrients more effectively, even as it uses up some extra calories – leading to a 14 percent increase in energy expenditure.
There are many ways in which this can be achieved. Intermittent fasting is one of them; with 16-h to 24-h fasts, for example. Intermittent calorie restriction is another; e.g., with a 1/3 and 2/3 calorie consumption pattern across two-day periods. Yet another is intermittent carbohydrate restriction, with other macronutrients kept more or less constant.
If the same amount of food is consumed, there is evidence suggesting that such practices would lead to body weight preservation with improved body composition – same body weight, but reduced fat mass. This is what the study by Anson and colleagues, mentioned earlier, suggested.
A 2005 study by Heilbronn and colleagues on alternate day fasting by humans suggested a small decrease in body weight (); although the loss was clearly mostly of fat mass. Interestingly, this study with nonobese humans suggested a massive decrease in fasting insulin, much like the mice study by Anson and colleagues.
Having said all of the above, there may be people who gain body fat by alternating between eating little and a lot. Why would that be? A possible reason is that when they eat a lot their caloric intake exceeds the increased energy expenditure.
Monday, July 16, 2012
The 14-percent advantage of eating little and then a lot: Is it real?
When you look at the literature on overfeeding, you see a number over and over again – 14 percent. That is approximately the increase in energy expenditure you get when you overfeed people; that is, when you feed people more calories that they need to maintain their current weight.
This phenomenon is related to another interesting one: the nonlinear increase in body weight and fat mass following overfeeding after a period starvation, illustrated by the top graph below from an article by Kevin Hall (). The data for the squares on the top graph is from the Minnesota Starvation Experiment (). The graph at the bottom is based mostly on the results of a simulation, and doesn’t clearly reflect the phenomenon.
Due to the significant amount of weight lost in what is called above the semistarvation stage (SS), the controlled refeeding period (CR) actually involved significant overfeeding. Nevertheless, weight was not gained right away, due to a sharp increase in energy expenditure. That is illustrated by the U-curve shape of the weight gain in response to overfeeding. Initially the gain is minimal, increasing over time, and continuing through the ad libitum refeeding stage (ALR).
Interestingly, overfeeding leads to increased energy expenditure almost immediately after it starts happening. It seems that even one single unusually big meal will significantly increase energy expenditure. Also, the 14 percent is usually associated with meals with a balanced amount of macronutrients. That percentage seems to go down if the balance is significantly shifted toward dietary fat (), probably because the metabolic “cost” of converting dietary fat into body fat is low. In other words, large meals with a lot of fat in them tend to cause a reduced increase in energy expenditure – less than 14 percent. Shifting the balance to protein appears to have the opposite effect, increasing energy expenditure even more, probably because protein is the jack-of-all-trades among macronutrients ().
The calorie surplus used in experiments where the 14 percent increase in energy expenditure is observed is normally around 1,000 calories, but the percentage seems to hold steady when people are overfed to different degrees () (). Let us assume that one is overfed 1,000 calories. What happens? About 140 calories are “lost” due to overfeeding.
What does this have to do with eating little, and then a lot, in an alternate way? It allows for some reasonable speculation, based on a simple pattern: when you alternate between underfeeding and overfeeding, you reduce food consumption for short period of time (usually less than 24 h), and then eat big, because you are hungry.
It is reasonable to assume, based on the empirical evidence on what happens during overfeeding, that the body reacts to “eating big” as it would to overfeeding, increasing energy expenditure by a certain amount. That increase leads to a reduction in the caloric value of the meals during overfeeding; a reduction of about 14 percent of the overfed amount.
But the body does not seem to significantly decrease energy expenditure if one reduces food consumption for a short period of time, such as 24 h. So you have the potential here for some steady fat loss without a reduction in caloric intake. Keeping a calorie intake up above a certain point is more important than many people think, because a calorie intake that is too low may lead to nutrient deficiencies (). This is possibly one of the reasons why carrying a bit of extra weight is associated with increased longevity in relatively sedentary populations ().
Is this 14-percent effect real, or just another mirage? If yes, what does it possibly translate into in terms of fat loss? More on these issues is coming in the next post.
This phenomenon is related to another interesting one: the nonlinear increase in body weight and fat mass following overfeeding after a period starvation, illustrated by the top graph below from an article by Kevin Hall (). The data for the squares on the top graph is from the Minnesota Starvation Experiment (). The graph at the bottom is based mostly on the results of a simulation, and doesn’t clearly reflect the phenomenon.
Due to the significant amount of weight lost in what is called above the semistarvation stage (SS), the controlled refeeding period (CR) actually involved significant overfeeding. Nevertheless, weight was not gained right away, due to a sharp increase in energy expenditure. That is illustrated by the U-curve shape of the weight gain in response to overfeeding. Initially the gain is minimal, increasing over time, and continuing through the ad libitum refeeding stage (ALR).
Interestingly, overfeeding leads to increased energy expenditure almost immediately after it starts happening. It seems that even one single unusually big meal will significantly increase energy expenditure. Also, the 14 percent is usually associated with meals with a balanced amount of macronutrients. That percentage seems to go down if the balance is significantly shifted toward dietary fat (), probably because the metabolic “cost” of converting dietary fat into body fat is low. In other words, large meals with a lot of fat in them tend to cause a reduced increase in energy expenditure – less than 14 percent. Shifting the balance to protein appears to have the opposite effect, increasing energy expenditure even more, probably because protein is the jack-of-all-trades among macronutrients ().
The calorie surplus used in experiments where the 14 percent increase in energy expenditure is observed is normally around 1,000 calories, but the percentage seems to hold steady when people are overfed to different degrees () (). Let us assume that one is overfed 1,000 calories. What happens? About 140 calories are “lost” due to overfeeding.
What does this have to do with eating little, and then a lot, in an alternate way? It allows for some reasonable speculation, based on a simple pattern: when you alternate between underfeeding and overfeeding, you reduce food consumption for short period of time (usually less than 24 h), and then eat big, because you are hungry.
It is reasonable to assume, based on the empirical evidence on what happens during overfeeding, that the body reacts to “eating big” as it would to overfeeding, increasing energy expenditure by a certain amount. That increase leads to a reduction in the caloric value of the meals during overfeeding; a reduction of about 14 percent of the overfed amount.
But the body does not seem to significantly decrease energy expenditure if one reduces food consumption for a short period of time, such as 24 h. So you have the potential here for some steady fat loss without a reduction in caloric intake. Keeping a calorie intake up above a certain point is more important than many people think, because a calorie intake that is too low may lead to nutrient deficiencies (). This is possibly one of the reasons why carrying a bit of extra weight is associated with increased longevity in relatively sedentary populations ().
Is this 14-percent effect real, or just another mirage? If yes, what does it possibly translate into in terms of fat loss? More on these issues is coming in the next post.
Monday, June 18, 2012
The lowest-mortality BMI: What is its relationship with fat-free mass?
Do overweight folks live longer? It is not uncommon to see graphs like the one below, from the Med Journal Watch blog (), suggesting that, at least as far as body mass index (BMI) is concerned (), overweight folks (25 < BMI < 30) seem to live longer. The graph shows BMI measured at a certain age, and risk of death within a certain time period (e.g., 20 years) following the measurement. The lowest-mortality BMI is about 26, which is in the overweight area of the BMI chart.

Note that relative age-adjusted mortality risk (i.e., relative to the mortality risk of people in the same age group), increases less steeply in response to weight variations as one becomes older. An older person increases the risk of dying to a lesser extent by weighing more or less than does a younger person. This seems to be particularly true for weight gain (as opposed to weight loss).
The table below is from a widely cited 2002 article by Allison and colleagues (), where they describe a study of 10,169 males aged 25-75. Almost all of the participants, ninety-eight percent, were followed up for many years after measurement; a total of 3,722 deaths were recorded.

Take a look at the two numbers circled in red. The one on the left is the lowest-mortality BMI not adjusting for fat mass or fat-free mass: a reasonably high 27.4. The one on the right is the lowest-mortality BMI adjusting for fat mass and fat-free mass: a much lower 21.6.
I know this may sound confusing, but due to possible statistical distortions this does not mean that you should try to bring your BMI to 21.6 if you want to reduce your risk of dying. What this means is that fat mass and fat-free mass matter. Moreover, all of the participants in this study were men. The authors concluded that: “…marked leanness (as opposed to thinness) has beneficial effects.”
Then we have an interesting 2003 article by Bigaard and colleagues () reporting on a study of 27,178 men and 29,875 women born in Denmark, 50 to 64 years of age. The table below summarizes deaths in this study, grouping them by BMI and waist circumference.

These are raw numbers; no complex statistics here. Circled in green is the area with samples that appear to be large enough to avoid “funny” results. Circled in red are the lowest-mortality percentages; I left out the 0.8 percentage because it is based on a very small sample.
As you can see, they refer to men and women with BMIs in the 25-29.9 range (overweight), but with waist circumferences in the lower-middle range: 90-96 cm for men and 74-82 cm for women; or approximately 35-38 inches for men and 29-32 inches for women.
Women with BMIs in the 18.5-24.9 range (normal) and the same or lower waists also died in small numbers. Underweight men and women had the highest mortality percentages.
A relatively small waist (not a wasp waist), together with a normal or high BMI, is an indication of more fat-free mass, which is retained together with some body fat. It is also an indication of less visceral body fat accumulation.

Note that relative age-adjusted mortality risk (i.e., relative to the mortality risk of people in the same age group), increases less steeply in response to weight variations as one becomes older. An older person increases the risk of dying to a lesser extent by weighing more or less than does a younger person. This seems to be particularly true for weight gain (as opposed to weight loss).
The table below is from a widely cited 2002 article by Allison and colleagues (), where they describe a study of 10,169 males aged 25-75. Almost all of the participants, ninety-eight percent, were followed up for many years after measurement; a total of 3,722 deaths were recorded.

Take a look at the two numbers circled in red. The one on the left is the lowest-mortality BMI not adjusting for fat mass or fat-free mass: a reasonably high 27.4. The one on the right is the lowest-mortality BMI adjusting for fat mass and fat-free mass: a much lower 21.6.
I know this may sound confusing, but due to possible statistical distortions this does not mean that you should try to bring your BMI to 21.6 if you want to reduce your risk of dying. What this means is that fat mass and fat-free mass matter. Moreover, all of the participants in this study were men. The authors concluded that: “…marked leanness (as opposed to thinness) has beneficial effects.”
Then we have an interesting 2003 article by Bigaard and colleagues () reporting on a study of 27,178 men and 29,875 women born in Denmark, 50 to 64 years of age. The table below summarizes deaths in this study, grouping them by BMI and waist circumference.

These are raw numbers; no complex statistics here. Circled in green is the area with samples that appear to be large enough to avoid “funny” results. Circled in red are the lowest-mortality percentages; I left out the 0.8 percentage because it is based on a very small sample.
As you can see, they refer to men and women with BMIs in the 25-29.9 range (overweight), but with waist circumferences in the lower-middle range: 90-96 cm for men and 74-82 cm for women; or approximately 35-38 inches for men and 29-32 inches for women.
Women with BMIs in the 18.5-24.9 range (normal) and the same or lower waists also died in small numbers. Underweight men and women had the highest mortality percentages.
A relatively small waist (not a wasp waist), together with a normal or high BMI, is an indication of more fat-free mass, which is retained together with some body fat. It is also an indication of less visceral body fat accumulation.
Monday, June 4, 2012
How to make white rice nutritious
One of the problems often pointed out about rice, and particularly about white rice, is that its nutrition content is fairly low. It is basically carbohydrates with some trace amounts of protein. A 100-g portion of cooked white rice will typically deliver 28 g of carbohydrates, with zero fiber, and 3 g of protein. The micronutrient content of such a portion leaves a lot to be desired when compared with fruits and vegetables, as you can see below (from Nutritiondata.com). Keep in mind that this is for 100 g of “enriched” white rice; the nutrients you see there, such as manganese, are added.
White rice is rice that has had its husk, bran, and germ removed. This prevents spoilage and thus significantly increases its shelf life. As it happens, it also significantly reduces both its nutrition and toxin content. White rice is one of the refined foods with the lowest toxin content.
Another interesting property of white rice is that it absorbs moisture to the tune of about 2.5 times its weight. That is, a 100-g portion of dry white rice will lead to a 250-g portion of edible white rice after cooking. This does not only dramatically decrease white rice’s glycemic load () compared with wheat-based products in general (with some exceptions, such as pasta), but also allows for white rice to be made into a highly nutritious dish.
If you slow cook almost anything in water, many of its nutrients will seep into the water. All you have to do is to then use that water (often called broth) to cook white rice in it, and you will end up with highly nutritious rice. Typically you will need twice as much broth as rice, cooked for about 15 minutes – e.g., 2 cups of broth for 1 cup of rice.
You can add meats to the white rice, such as pulled chicken or shrimp; add some tomato sauce to that and you’ll make it a chicken or shrimp risotto. You can also add vegetables to the rice. If you want your rice to have something like an al dente consistency, I recommend doing these after the rice is ready; i.e., after you cooked it in the broth.
For the white rice-based dish below I used a broth from about two hours of slow cooking of diced vegetables; namely red bell peppers, carrots, celery, onions, and cabbage. After cooking the rice for 15 minutes, and letting it "sit" for a while (another 15 minutes with the pan covered), I also added the vegetables to it.
As a side note, the cabbage and onion tend to completely dissolve after 1 h or so of slow cooking. The added vegetables give the dish quite a nutritional punch. For example, the cabbage alone seems to be a great source of vitamin C (which is not completely destroyed by the slow cooking), the anti-inflammatory amino acid glutamine, and the DNA repair-promoting substance known as indole-3-carbinol ().
The good folks over at the Highbrow Paleo group on Facebook () had a few other great ideas posted in response to my previous post on the low glycemic load of white rice (), such as cooking white rice in bone broth (thanks Derrick!).
White rice is rice that has had its husk, bran, and germ removed. This prevents spoilage and thus significantly increases its shelf life. As it happens, it also significantly reduces both its nutrition and toxin content. White rice is one of the refined foods with the lowest toxin content.
Another interesting property of white rice is that it absorbs moisture to the tune of about 2.5 times its weight. That is, a 100-g portion of dry white rice will lead to a 250-g portion of edible white rice after cooking. This does not only dramatically decrease white rice’s glycemic load () compared with wheat-based products in general (with some exceptions, such as pasta), but also allows for white rice to be made into a highly nutritious dish.
If you slow cook almost anything in water, many of its nutrients will seep into the water. All you have to do is to then use that water (often called broth) to cook white rice in it, and you will end up with highly nutritious rice. Typically you will need twice as much broth as rice, cooked for about 15 minutes – e.g., 2 cups of broth for 1 cup of rice.
You can add meats to the white rice, such as pulled chicken or shrimp; add some tomato sauce to that and you’ll make it a chicken or shrimp risotto. You can also add vegetables to the rice. If you want your rice to have something like an al dente consistency, I recommend doing these after the rice is ready; i.e., after you cooked it in the broth.
For the white rice-based dish below I used a broth from about two hours of slow cooking of diced vegetables; namely red bell peppers, carrots, celery, onions, and cabbage. After cooking the rice for 15 minutes, and letting it "sit" for a while (another 15 minutes with the pan covered), I also added the vegetables to it.
As a side note, the cabbage and onion tend to completely dissolve after 1 h or so of slow cooking. The added vegetables give the dish quite a nutritional punch. For example, the cabbage alone seems to be a great source of vitamin C (which is not completely destroyed by the slow cooking), the anti-inflammatory amino acid glutamine, and the DNA repair-promoting substance known as indole-3-carbinol ().
The good folks over at the Highbrow Paleo group on Facebook () had a few other great ideas posted in response to my previous post on the low glycemic load of white rice (), such as cooking white rice in bone broth (thanks Derrick!).
Monday, May 21, 2012
Rice consumption and health
Carbohydrate-rich foods lead to the formation of blood sugars after digestion (e.g., glucose, fructose), which are then used by the liver to synthesize liver glycogen. Liver glycogen is essentially liver-stored sugar, which is in turn used to meet the glucose needs of the human brain – about 5 g/h for the average person.
When one thinks of the carbohydrate content of foods, there are two measures that often come to mind: the glycemic index and the glycemic load. Of these two, the first, the glycemic index, tends to get a lot more attention. Some would argue that the glycemic load is a lot more important, and that rice, as consumed in Asia, may provide a good illustration of that importance.
A 100-g portion of cooked rice will typically deliver 28 g of carbohydrates, with zero fiber, and 3 g of protein. By comparison, a 100-g portion of white Italian bread will contain 54 g of carbohydrates, with 4 g of fiber, and 10 g of protein – the latter in the form of gluten. A 100-g portion of baked white potato will have 21 g of carbohydrates, with 2 g of fiber, and 2 g of protein.
As you can see above, the amount of carbohydrate per gram in white rice is about half that of white bread. One of the reasons is that the water content in rice, as usually consumed, is comparable to that in fruits. Not surprisingly, rice’s glycemic load is 15 (medium), which is half the glycemic load of 30 (high) of white Italian bread. These refer to 100-g portions. The glycemic load of 100 g of baked white potato is 10 (low).
The glycemic load of a portion of food allows for the estimation of how much that portion of food raises a person's blood glucose level; with one unit of glycemic load being equivalent to the blood glucose effect of consumption of one gram of glucose.
Two common denominators between hunter-gatherer groups that consume a lot of carbohydrates and Asian populations that also consume a lot of carbohydrates are that: (a) their carbohydrate consumption apparently has no negative health effects; and (b) they consume carbohydrates from relatively low glycemic load sources.
The carbohydrate-rich foods consumed by hunter-gatherers are predominantly fruits and starchy tubers. For various Asian populations, it is predominantly white rice. As noted above, the water content of white rice, as usually consumed by Asian populations, is comparable to that of fruits. It also happens to be similar to that of cooked starchy tubers.
An analysis of the China Study II dataset, previously discussed here, suggests that widespread replacement of rice with wheat flour may have been a major source of problems in China during the 1980s and beyond ().
Even though rice is an industrialized seed-based food, the difference between its glycemic load and those of most industrialized carbohydrate-rich foods is large (). This applies to rice as usually consumed – as a vehicle for moisture or sauces that would otherwise remain on the plate. White rice combines this utilitarian purpose with a very low anti-nutrient content.
It is often said that white rice’s nutrient content is very low, but this problem can be easily overcome – a topic for the next post.
(Source: Wikipedia)
When one thinks of the carbohydrate content of foods, there are two measures that often come to mind: the glycemic index and the glycemic load. Of these two, the first, the glycemic index, tends to get a lot more attention. Some would argue that the glycemic load is a lot more important, and that rice, as consumed in Asia, may provide a good illustration of that importance.
A 100-g portion of cooked rice will typically deliver 28 g of carbohydrates, with zero fiber, and 3 g of protein. By comparison, a 100-g portion of white Italian bread will contain 54 g of carbohydrates, with 4 g of fiber, and 10 g of protein – the latter in the form of gluten. A 100-g portion of baked white potato will have 21 g of carbohydrates, with 2 g of fiber, and 2 g of protein.
As you can see above, the amount of carbohydrate per gram in white rice is about half that of white bread. One of the reasons is that the water content in rice, as usually consumed, is comparable to that in fruits. Not surprisingly, rice’s glycemic load is 15 (medium), which is half the glycemic load of 30 (high) of white Italian bread. These refer to 100-g portions. The glycemic load of 100 g of baked white potato is 10 (low).
The glycemic load of a portion of food allows for the estimation of how much that portion of food raises a person's blood glucose level; with one unit of glycemic load being equivalent to the blood glucose effect of consumption of one gram of glucose.
Two common denominators between hunter-gatherer groups that consume a lot of carbohydrates and Asian populations that also consume a lot of carbohydrates are that: (a) their carbohydrate consumption apparently has no negative health effects; and (b) they consume carbohydrates from relatively low glycemic load sources.
The carbohydrate-rich foods consumed by hunter-gatherers are predominantly fruits and starchy tubers. For various Asian populations, it is predominantly white rice. As noted above, the water content of white rice, as usually consumed by Asian populations, is comparable to that of fruits. It also happens to be similar to that of cooked starchy tubers.
An analysis of the China Study II dataset, previously discussed here, suggests that widespread replacement of rice with wheat flour may have been a major source of problems in China during the 1980s and beyond ().
Even though rice is an industrialized seed-based food, the difference between its glycemic load and those of most industrialized carbohydrate-rich foods is large (). This applies to rice as usually consumed – as a vehicle for moisture or sauces that would otherwise remain on the plate. White rice combines this utilitarian purpose with a very low anti-nutrient content.
It is often said that white rice’s nutrient content is very low, but this problem can be easily overcome – a topic for the next post.
Monday, May 7, 2012
The 2012 Arch Intern Med red meat-mortality study: The “protective” effect of smoking
In a previous post () I used WarpPLS () to analyze the model below, using data reported in a recent study looking at the relationship between red meat consumption and mortality. The model below shows the different paths through which smoking influences mortality, highlighted in red. The study was not about smoking, but data was collected on that variable; hence this post.
When one builds a model like the one above, and tests it with empirical data, the person does something similar to what a physicist would do. The model is a graphical representation of a complex equation, which embodies the beliefs of the modeler. WarpPLS builds the complex equation automatically for the user, who would otherwise have to write it down using mathematical symbols.
The results yielded by the complex equation, partly in the form of coefficients of association for direct relationships (the betas next to the arrows), have a meaning. Some may look odd, and require novel interpretations, much in the same way that odd results from an equation describing planetary motions may have led to the development of the theory of black holes.
Nothing is actually "proven" by the results. They are part of the long and painstaking process we call "research". To advance new knowledge, one needs a lot more than a single study. Darwin's theory of evolution is still being tested. Based on various tests and partial refutations, it has itself evolved a great deal since its original formulation.
One set of results that are generated based on the model above by WarpPLS, in addition to coefficients for direct relationships, are coefficients of association called "total effects". They aggregate all of the effects, via multiple paths, between each pair of variables. Below is a table of total effects, with the total effects of smoking on diabetes incidence and overall mortality highlighted in red.
As you can see, the total effects of smoking on diabetes incidence and overall mortality are negative, but small enough to be considered insignificant. This is interesting, because smoking is definitely not health-promoting. Among hunter-gatherers, who often smoke tobacco, it increases the incidence of various types of cancer (). And it may be at the source of many of the health problems suggested by analyses on the China Study II data ().
So what are these results telling us? They tell us that smoking has an intermediate protective effect, very likely associated with its anorexic effect. Smoking is an appetite suppressor. Its total effect on food intake is negative, and strong. As we can see from the table of total effects, just below the two numbers highlighted in red, the total effect of smoking on food intake is -0.356.
Still, it looks like smoking is nearly as bad as overeating to the point of becoming obese (), in terms of its overall effect on health. Otherwise we would see a positive total effect on overall mortality of comparable strength to the negative total effect on food intake.
Smoking may make one eat less, but it ends up hastening one’s demise through different paths.
When one builds a model like the one above, and tests it with empirical data, the person does something similar to what a physicist would do. The model is a graphical representation of a complex equation, which embodies the beliefs of the modeler. WarpPLS builds the complex equation automatically for the user, who would otherwise have to write it down using mathematical symbols.
The results yielded by the complex equation, partly in the form of coefficients of association for direct relationships (the betas next to the arrows), have a meaning. Some may look odd, and require novel interpretations, much in the same way that odd results from an equation describing planetary motions may have led to the development of the theory of black holes.
Nothing is actually "proven" by the results. They are part of the long and painstaking process we call "research". To advance new knowledge, one needs a lot more than a single study. Darwin's theory of evolution is still being tested. Based on various tests and partial refutations, it has itself evolved a great deal since its original formulation.
One set of results that are generated based on the model above by WarpPLS, in addition to coefficients for direct relationships, are coefficients of association called "total effects". They aggregate all of the effects, via multiple paths, between each pair of variables. Below is a table of total effects, with the total effects of smoking on diabetes incidence and overall mortality highlighted in red.
As you can see, the total effects of smoking on diabetes incidence and overall mortality are negative, but small enough to be considered insignificant. This is interesting, because smoking is definitely not health-promoting. Among hunter-gatherers, who often smoke tobacco, it increases the incidence of various types of cancer (). And it may be at the source of many of the health problems suggested by analyses on the China Study II data ().
So what are these results telling us? They tell us that smoking has an intermediate protective effect, very likely associated with its anorexic effect. Smoking is an appetite suppressor. Its total effect on food intake is negative, and strong. As we can see from the table of total effects, just below the two numbers highlighted in red, the total effect of smoking on food intake is -0.356.
Still, it looks like smoking is nearly as bad as overeating to the point of becoming obese (), in terms of its overall effect on health. Otherwise we would see a positive total effect on overall mortality of comparable strength to the negative total effect on food intake.
Smoking may make one eat less, but it ends up hastening one’s demise through different paths.
Monday, April 23, 2012
Hunger is your best friend: It makes natural foods taste delicious and promotes optimal nutrient partitioning
One of the biggest problems with modern diets rich in industrial foods is that they promote unnatural hunger patterns. For example, hunger can be caused by hypoglycemic dips, coupled with force-storage of fat in adipocytes, after meals rich in refined carbohydrates. This is a double-edged post-meal pattern that is induced by, among other things, abnormally elevated insulin levels. The resulting hunger is a rather unnatural type of hunger.
By the way, I often read here and there, mostly in blogs, that “insulin suppresses hunger”. I frankly don’t know where this idea comes from. What actually happens is that insulin is co-secreted with a number of other hormones. One of those, like insulin also secreted by the beta-cells in the pancreas, is amylin – a powerful appetite suppressor. Amylin deficiency leads to hunger even after a large carbohydrate-rich meal, when insulin levels are elevated.
Abnormally high insulin levels – like those after a “healthy” breakfast of carbohydrate-rich cereals, pancakes etc. – lead to abnormal blood glucose dips soon after the meal. What I am talking about here is a fall in glucose levels that is considerable, and that also happens very fast – illustrated by the ratio between the lengths of the vertical and horizontal black lines on the figure below, from a previous post ().
Those hypoglycemic dips induce hunger, because the hormonal changes necessary to apply a break to the fall in glucose levels (which left unchecked would lead to death) leave us with a hormonal mix that ends up stimulating hunger, in an unnatural way. At the bottom of those dips, insulin levels are much lower than before. I am not talking about diabetics here. I am talking about normoglycemic folks, like the ones whose glucose levels are show on the figure above.
On a diet primarily of natural foods, or foods that are not heavily modified from their natural state, hunger patterns tend to be better synchronized with nutrient deficiencies. This is one of the main advantages of a natural foods diet. By nutrients, I do not mean only micronutrients such as vitamins and minerals, but also macronutrients such as amino and fatty acids.
On a natural diet, nutrient deficiencies should happen regularly. Our bodies are designed for sporadic nutrient intake, remaining most of the time in the fasted state. Human beings are unique in that they have very large brains in proportion to their overall body size, brains that run primarily on glucose – the average person’s brain consumes about 5 g/h of glucose. This latter characteristic makes it very difficult to extrapolate diet-based results based on other species to humans.
As hunger becomes better synchronized with nutrient deficiencies, it should promote optimal nutrient partitioning. This means that, among other things: (a) you should periodically feel hungry for different types of food, depending on your nutrient needs at that point in time; (b) if you do weight training, and fell hungry, some muscle gain should follow; and (c) if you let hunger drive food consumption, on a diet of predominantly natural foods, body fat levels should remain relatively low.
In this sense, hunger becomes your friend – and the best spice!
By the way, I often read here and there, mostly in blogs, that “insulin suppresses hunger”. I frankly don’t know where this idea comes from. What actually happens is that insulin is co-secreted with a number of other hormones. One of those, like insulin also secreted by the beta-cells in the pancreas, is amylin – a powerful appetite suppressor. Amylin deficiency leads to hunger even after a large carbohydrate-rich meal, when insulin levels are elevated.
Abnormally high insulin levels – like those after a “healthy” breakfast of carbohydrate-rich cereals, pancakes etc. – lead to abnormal blood glucose dips soon after the meal. What I am talking about here is a fall in glucose levels that is considerable, and that also happens very fast – illustrated by the ratio between the lengths of the vertical and horizontal black lines on the figure below, from a previous post ().
Those hypoglycemic dips induce hunger, because the hormonal changes necessary to apply a break to the fall in glucose levels (which left unchecked would lead to death) leave us with a hormonal mix that ends up stimulating hunger, in an unnatural way. At the bottom of those dips, insulin levels are much lower than before. I am not talking about diabetics here. I am talking about normoglycemic folks, like the ones whose glucose levels are show on the figure above.
On a diet primarily of natural foods, or foods that are not heavily modified from their natural state, hunger patterns tend to be better synchronized with nutrient deficiencies. This is one of the main advantages of a natural foods diet. By nutrients, I do not mean only micronutrients such as vitamins and minerals, but also macronutrients such as amino and fatty acids.
On a natural diet, nutrient deficiencies should happen regularly. Our bodies are designed for sporadic nutrient intake, remaining most of the time in the fasted state. Human beings are unique in that they have very large brains in proportion to their overall body size, brains that run primarily on glucose – the average person’s brain consumes about 5 g/h of glucose. This latter characteristic makes it very difficult to extrapolate diet-based results based on other species to humans.
As hunger becomes better synchronized with nutrient deficiencies, it should promote optimal nutrient partitioning. This means that, among other things: (a) you should periodically feel hungry for different types of food, depending on your nutrient needs at that point in time; (b) if you do weight training, and fell hungry, some muscle gain should follow; and (c) if you let hunger drive food consumption, on a diet of predominantly natural foods, body fat levels should remain relatively low.
In this sense, hunger becomes your friend – and the best spice!