Occasionally I get emails from people experiencing odd fluctuations in health markers, and trying to figure out what is causing those fluctuations. Spikes in LDL cholesterol without any change in diet seem to be a common occurrence, especially in men.
LDL cholesterol is a reflection of many things. It is one of the least useful measures in standard lipid profiles, as a predictor of future health problems. Nevertheless, if one’s diet is not changing, whether it is high or low in fat, significant fluctuations in LDL cholesterol may signal a change in inflammatory status. Generally speaking, the more systemic inflammation, the higher is the measured LDL cholesterol.
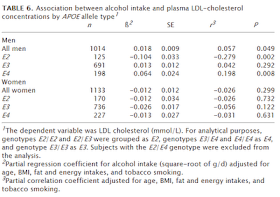
Corella and colleagues (2001) looked into alcohol consumption and its effect on LDL cholesterol, as part of the Framingham Offspring Study. They split the data into three genotypes, which are allele combinations. Alleles are genes variations; that is, they are variations in the sections of DNA that have been identified as coding for observable traits. The table below summarizes what they have found. Take a look at the last two columns on the right.
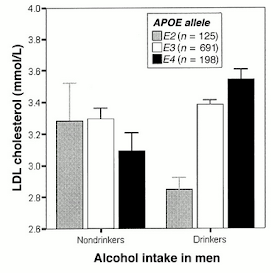
As you can see, for men with the E2 genotype, alcohol consumption significantly decreases LDL cholesterol. For men with the E4 genotype, alcohol consumption significantly increases LDL cholesterol. No significant effects were observed in women. The figure below illustrates the magnitude of the effects observed in men.
On average, alcohol consumption was moderate, around 15 g per day, and did not vary significantly based on genotype. This is important. Otherwise one could argue that a particular genotype predisposed individuals to drink more, which would be a major confounder in this study. Other confounders were also ruled out through multivariate controls - e.g., fat and calorie intake, and smoking.
Alcohol consumption in moderation seems, on average, to be beneficial. But for some individuals, particularly men with a certain genotype, it may be advisable to completely abstain from alcohol consumption. Who are those folks? They are the ones for whom LDL cholesterol goes up significantly following moderate alcohol consumption.
This comment has been removed by the author.
ReplyDeleteHow do these people know they have LDL spikes? Most people don't get LDL measured that often, and there are no home LDL meters.
ReplyDeleteA spike is merely a sharp interruption of a trend. The trend could be over the course of years. One needn't test often to notice a spike. (But once you notice the spike, you might be tempted to increase the frequency of testing;)
ReplyDeleteHey Ned,
ReplyDeleteThis is interesting. However, if taken alone, it seems very unconvincing. Are there any supportive data either showing a biochemical/molecular mechanism or showing in a clinical trial that this occurs when subjects are randomized by genotype?
My view of these types of associations is that, in general, researchers will practice post-hoc data mining splicing things many ways by alternative subgroup analysis and then report a small portion of it, leading to "positive" findings where the findings were otherwise null, thus allowing publication of what is really negative data so as to not throw grant money in the toilet.
Chris
Hi Gretchen. Even the calculated LDL-C from standard lipid profiles will be enough here.
ReplyDeleteHi Gregory. I get as many measurements as I can done on a regular basis though my insurance. One cannot go wrong with more rather than less information. The key is to try to understand what the numbers mean, from a big picture perspective, and not to act too quickly.
ReplyDeleteHi Chris. The process you described is how most research is done, and how most truly novel discoveries are made.
ReplyDeleteAs for the results of this study, I am not very surprised by them. Alcohol has been around for some time, a few thousand years, enough to play a role in selection. But this has probably been restricted to some groups and not to others – e.g., the anthropological record suggests that most isolated hunter-gatherers have not consumed alcohol.
So you’d expect to see marked differences in health markers based on genotype in modern humans, especially in groups with mixed backgrounds like the Framingham folks.
One arguably very interesting result of this study is the general lack of an effect in women; the reasons have already been discussed here, on this post:
http://bit.ly/fL8Rpc
Hi Ned,
ReplyDeleteI agree that this is how most research is done and that it can theoretically lead to new discoveries, but surely you agree that if someone looks at ten different ways of subgrouping data where there is no association otherwise and finds that one of them leads to significant results it could quite easily be spurious, no?
I don't find the results implausible, I'm just wondering if you know of any supportive data that can corroborate this. I think the appropriate way to treat post-hoc subgroup analysis in epidemiology is to look for the association in a new population where the study is designed specifically for that purpose. To provide evidence of causality, of course, I'd like to see some mechanistic or clinical data.
I'm not suggesting the results are wrong, just asking if you know of any data corroborating them.
By the way I cited your shrinkage post in my latest post. Keep up the good work; I look forward to listening to your interview.
Chris
Hi Chris. I have only anecdotal evidence supporting these findings. In fact, what prompted me to put out this post now were two HealthCorrelator for Excel (HCE) users, who sent me their HCE analyses and raw datasets recently. I’ve redone the analyses myself, and they pointed at alcohol consumption as the main likely cause of not only high LDL-C but also elevated trigs and other problems.
ReplyDeleteThanks for the referral. I also mentioned you, I hope correctly, in my interview with Jimmy Moore. This was related to a point that you made (I believe) about industrial seed oils leading to some short-term improvements in health markers due to their high vitamin E content, even though long-term they may have quite the opposite effect.
Ned, my point was that most people don't measure LDL that often at all, not referring to real measurement vs calculated.
ReplyDeleteAnd so many things affect lipid levels.
I guess I have a different meaning for "spike." To me a spike is something that goes high quickly and then comes down quickly.
"One cannot go wrong with more rather than less information."
ReplyDeleteI understand what you mean, and applaud the sentiment in principle. But I'm not sure I agree--at least from a public health standpoint in country where health decisions are most often driven by the misconceptions of doctors.
For example, the recent studies of PSA testing suggest that knowing PSA does more harm than good; it may prolong life in a very small section of the public, but it also results in an incredible number of unneeded surgical interventions that result in a wide array of disabilities (and, yes, additional mortality) in men ho would have died of other causes long before prostate cancer would have made a difference in their lives.
More to your point, consider the matter of lipid profiles. If you combine all of the bad dietary advice dispensed by doctors in an effort to lower cholesterol levels, coupled with all the damage caused by statins (I have a friend who has had serious episodes of amnesia from Lipitor; his doctor agrees that the statin is the cause, but these eisodes of memory loss might be worth it to keep his cholesterol low)...and I wonder if more information is intrinsically better.
If you are extremely well-informed, quite skeptical, able to resist pressure from "experts," and can find a doctor that listens to you, then more information might be better.
Hi David. I should say that I’d avoid invasive exams.
ReplyDeleteNow, to your point, what’s really important for people in general to understand is that they are in charge as far as their health is concerned.
The patient does not have to agree with the doctor, or vice-versa, as long as both are willing to communicate.
But to communicate patients have to read, and know themselves, for which numbers help a lot.
I know a lot of guys who are experts on how their cars work, but know next to nothing about how their bodies work.
You hit the nail on the head.
ReplyDeleteOne of the biggest problems we face, I think, is the rise of HMOs, which often try to limit the nature of the doctor-patient relationship.
To give an example from my own experience: I used to be on Kaiser. When I was overweight and diagnosed with hypertension, they insisted I begin taking antihypertensives. Okay, fair enough. But after getting the results from my bloodwork, the computer system automatically generated sevral pages of patient handouts with specific recommendations, including:
1) Following a strict low-fat diet;
2) Beginning statins immediately;
3) Cutting my salt intake by half (without first determining my baseline salt intake);
4) Beginning a program of low-intensity endurance exercise.
I refused the first two. (I foolishly followed the third, for a while, and combined with exercise I later had a convulsion casued by--you guessed it--low sodium.)
But I digress. The problem is that public health mythology overrides the doctor-patient interaction.
In Michael Moore's movie SICKO, he interviews a London doctor who explains that under the NIH, his bonus pay for the year is partly determined by achieving "health outcomes." He notes that he gets paid more every time he lowers a patient's cholesterol.
Moore of course presents this as something we need to institute in the US...
Hi Ned
ReplyDeleteYou say "On average, alcohol consumption was moderate, around 15 g per day" Did you mean 150g/day? 15g seems much too low.
You say "Alcohol consumption in moderation seems, on average, to be beneficial." How does that follow from the study? Longevity vs LDL appears to be a U shaped distribution from observational studies of health outcomes.
I wonder if you have more analysis of the LDL Cholesterol!
ReplyDelete