Calcidiol is a pre-hormone that is produced based on vitamin D3 in the liver. Blood concentration of calcidiol is considered to be a reliable indicator of vitamin D status. In the research literature, calcidiol is usually referred to as 25-Hydroxyvitamin or 25(OH)D. Calcidiol is converted in the kidneys into calcitriol, which is the active form of vitamin D.
The table below (from: Vieth, 1999; full reference at the end of this post; click on it to enlarge), shows the average blood vitamin D levels of people living or working in sun-rich environments. To convert from nmol/L to ng/mL, divide by 2.496. For example, 100 nmol/L = 100 / 2.496 ng/mL = 40.1 ng/mL. At the time of this writing, Vieth (1999) had over 1500 citations on Google Scholar, and probably a large number as well on Web of Science. This article has had, and continues having, a high impact among researchers.
The maximum average level of blood (or serum) vitamin D shown in the table is 163 nmol/L (65 ng/mL). Given that the human body produces vitamin D naturally from sunlight, it is reasonable to assume that those blood vitamin D levels are not yet at the toxic range. In fact, one of the individuals, a farmer in Puerto Rico, had a level of 225 nmol/L (90 ng/mL). That individual had no signs of toxicity.
Several studies show that pre-sunburn full-body exposure to sunlight is equivalent to an oral vitamin D intake of approximately 250 µg (10,000 IU).
In spite of claims to the contrary, vitamin D production based on sunlight does not cease after 40 years of age or so. Studies reviewed by Vieth suggest that among the elderly (i.e., those aged 65 or above) pre-sunburn full-body exposure to sunlight is equivalent to an oral vitamin D intake of 218 µg (8,700 IU).
Sunlight-induced vitamin D production does seem to decrease with age, but not dramatically.
Post-sunburn sunlight exposure does not increase vitamin D production. Since each person is different, a good rule of thumb to estimate the number of minutes of sunlight exposure needed to maximize vitamin D production is the number of minutes preceding sunburn. For a light-skinned person, this can be as little as 7 minutes.
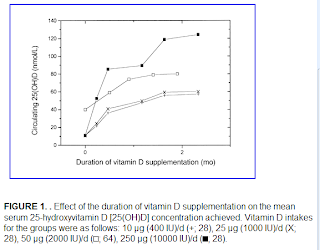
Vitamin D accumulation in the body follows a battery-like pattern, increasing and decreasing gradually. The figure below, from Vieth’s article, shows the gradual increase in blood vitamin D concentrations following the start of daily supplementation. This suggests that levels start to plateau at around 1 month, with higher levels reaching a plateau after 2 months.
While sunlight exposure does not lead to toxic levels of vitamin D, oral intake may. Below is a figure, also from Vieth’s article, that plots blood levels of vitamin D against oral intake amounts. The X’s indicate points at which intoxication symptoms were observed. While typically intoxication starts at the 50,000 IU intake level, one individual displayed signs of intoxication at 10,000 IU. That individual received a megadose that was supposed to provide vitamin D for an extended period of time.
Non-toxic levels of 10,000 IU are achieved naturally through sunlight exposure. This applies to modern humans and probably our Paleolithic ancestors. Yet, modern humans normally limit their sun exposure and intake of vitamin D to levels (400 IU) that are only effective to avoid osteomalacia, the softening of the bones due to poor mineralization.
Very likely the natural production of 10,000 IU based on sunlight was adaptive in our evolutionary past, and also necessary for good health today. This is consistent with the many reports of diseases associated with chronic vitamin D deficiency, even at levels that avoid osteomalacia. Among those diseases are: hypertension, tuberculosis, various types of cancer, gingivitis, multiple sclerosis, chronic inflammation, seasonal affective disorder, and premature senescence.
Reference:
Reinhold Vieth (May 1999). Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. American Journal of Clinical Nutrition, Vol. 69, No. 5, 842-856.
Sunday, September 23, 2018
Subscribe to:
Post Comments (Atom)



15 comments:
"This is consistent with the many reports of diseases associated with chronic vitamin D deficiency"
Please bear in mind that the data was the same for antioxidants; low levels were found to be strongly associated with disease. When they did the trials, lo and behold, their hapless human guinea pigs started to die, the excess was so great in several cases that the trials were halted.
The evidence against antioxidant (and other vitamins like folic acid) supplementation has been mounting up inexorably, what makes you think vitamin D will be different?
'Evolutionary flaws - or are they?' ( G. Cochran)
"You see, although wandering into suboptimal solutions is certainly possible, you can be sure to see slick, polished, tested and robust
implementations of those basically suboptimal designs. Almost always, given an environment that isn't too different fron the ancestral one, those designs will work just as well as they can, which is usually pretty damn well. And if they work well in anyone, you should expect to see them work well in almost everyone.
"A thousand generations of humans in Northern Europe were naturaly selected for maximum fitness in UVB-less winters. It follows that the vitamin D system in their descendants is calibrated and optimized for the summer rise and winter fall in vitamin D levels at northern latitudes. I trust evolution to find the 'sweet spot' for the vitamin D system , ie the setting that keeps me healthy (and looking that way) for as long as possible.
Implicit in the talk of vitamin D insufficiency is that there is a best vitamin D level applicable to everyone and everyone should supplement until it is reached. I just doesn't work that way, levels reached by supplementation do not bring the expected benefits for antioxidants ect. It will take longer for the deleterious effect of vitamin D supplementation to be discovered because it mimic aging and aging is a subtle process.
The end result will be the same: benighted amateur nutritionists putting their lives into fast forward
Ken:
I think you are right in keeping a skeptical attitude. So do I. But there is mounting evidence that: (a) vitamin D deficiency is associated with a host of diseases; and (b) the levels of vitamin D that we obtain through dietary sources are much lower than through exposure to sunlight.
On point (b) above, exposure to sunlight leads to vitamin D levels that are 2,500 percent (10,000 IU / 400 IU) higher than via dietary sources, even after fortification. The situation with antioxidants (e.g., glutathione, vitamins C and E, various enzymes) is very, very different.
I still have my doubts about oral supplementation of vitamin D. Personally pre-sunburn sunlight exposure is a preferable source of vitamin D; living in South Texas makes it possible during most of the year. But my review of the research so far suggests that vitamin D deficiency is more of a problem than many people think.
I will keep reviewing the data with an open mind though. Thanks for the references. I will read them again later.
Hi Ned,
I posted this over on the Heart Scan Blog, but would be curious to hear your take on these studies:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2892544/?tool=pmcentrez&report=abstract
http://cancerres.aacrjournals.org/cgi/content/full/66/20/9802
http://cancerres.aacrjournals.org/cgi/content/abstract/69/4/1439
http://aje.oxfordjournals.org/cgi/content/abstract/kwq114
Last year my 25-hydroxy was 19 ng/ml, since then I've been taking 4000iu a day in the hopes to get it around 75ng/ml. But with those studies showing a correlation of high vitamin d and super dangerous cancers (like pancreatic), perhaps supplementing vit-d3 is NOT a no-brainer! Perhaps vitamin d via sunlight is the only safe way to go (since potentially the other photoproducts are necessary (tachysterol, lumisterol, etc )
Hi enliteneer.
I think that pre-sunburn sunlight exposure is preferable, if possible. If not, supplementation may be advisable, but people should set their expectations about ranges of D levels more realistically. One would expect most (68 percent) of the population to be in the 42 to 63 ng/mL range at an intake of 10,000 IU/d.
As for the studies you linked, the evidence is a bit mixed, and none provides anything close to conclusive evidence that high vitamin D levels may cause cancer, in my opinion. The first shows some evidence among Asians, but that may be confounded by other factors (upper GI cancer is more common among Asians, and genetic and dietary factors have been proposed). One of the links actually discusses a protective effect.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2892544/?tool=pmcentrez&report=abstract
"... circulating 25(OH)D concentration was not significantly associated with upper GI cancer risk. Subgroup analysis by race showed that among Asians, but not Caucasians, lower concentrations of 25(OH)D (<25 nmol/L) were associated with a statistically significant decreased risk of upper GI cancer ..."
http://cancerres.aacrjournals.org/cgi/content/full/66/20/9802
"... in a recent, well-conducted prospective study among members of the Health Professionals Follow-up Study (HPFS) cohort by Giovannucci et al. ( 10), vitamin D exposure (based on multiple determinants of vitamin D status) was inversely associated with pancreatic cancer risk ..."
http://cancerres.aacrjournals.org/cgi/content/abstract/69/4/1439
"... Vitamin D concentrations were not associated with pancreatic cancer overall (highest versus lowest quintile, >82.3 versus <45.9 nmol/L: OR, 1.45; 95% CI, 0.66–3.15; P trend = 0.49). However, positive associations were observed among subjects with low estimated annual residential solar UBV exposure ..."
http://healthcorrelator.blogspot.com/2010/02/vitamin-d-levels-sunlight-age-and.html
"... there was no association between 25(OH)D concentration and disease risk, after adjustment for body mass index ...'
This last one is very telling - with BMI is controlled for, no association is found. Obesity is strongly associated with cancer risk, for almost all types of cancer. The association is very, very strong:
http://healthcorrelator.blogspot.com/2010/04/body-mass-index-and-cancer-deaths-in.html
great post!
"In spite of claims to the contrary, vitamin D production based on sunlight does not cease after 40 years of age or so."
well, in my case, it clearly did shut down. i'm 41, and despite sunbathing at least for an hour 3x a week w/o sunscreen during the UV intensive hours of the day PLUS taking 5'000IU D3 per day at the same time, i remained *exactly* at the same deficient level (60nmol) as before. and it has nothing to do with latitude or skin type etc. i checked all those factors. wrt to the 5kIU supplement, i think it's possible that i didn't absorb it properly due to my suspected gluten intolerance (damaged vilii), but why did the sun not work then? what i read is that at age 40, one only generates about 50% of the D compared to a 20y old. i tend to believe that, because the same just happened with my brother (46y). several month of intensive sunbathing, but still clearly deficient (even lower than me, 50nmol). so how do you explain THAT? ;)
Hi qualia.
There are quite a few possible reasons for that. As with almost any human trait, vit D production based on sun exposure can be affected by a number of factors.
For example, vit D is produced by the skin based on cholesterol. So low cholesterol levels can have a negative effect. A lot of people aged 40 and above take statins to reduce their cholesterol levels, an ill-advised strategy on many grounds. This may impair vit D production.
Obesity and overweight also affect blood vit D levels, due to what some researchers call the "hoarding" effect that body fat has on fat-soluble vitamins. Vit D is a fat-soluble vitamin.
Liver abnormalities can also affect vit D levels, as vitamin D3 (cholecalciferol) is hydroxylated in the liver to produce 25-hydroxycholecalciferol (calcidiol). Many things can cause liver abnormalities, and very few of these abnormalities show up in typical tests (e.g., liver enzymes). The main common trait is that these things are "man-made". They include man-made foods, such as table sugar and industrial cooking oils, and drugs such as statins.
Btw, a one-hour sun exposure, when the sun is high, is a very long exposure for almost anybody. Most people would develop skin damage and/or sunburns if they stayed in the sun for that long. I'm not sure if that affects vit D production, but it might, since the skin is the "organ" involved, and it is being damaged.
Vitamin D is one of the only vitamins produced naturally by the body. Vitamin D is unique because it is derived both from sunlight and foods.
Vitamin D is very important to us
and that is why we have to include vitamin rich food in our day to day life. Sun light in the morning is a good and natural source of sunlight.
I have read your article completely really it is very nice and informative. it explains almost all the information related to vitamin D......
Smith ALan
I think that the vitamin D is one of the best help to the body, I would like too read a little more about it!!
Hello, i think that this post is very good, i would like to read more about it
I just got my blood drawn. I am 79 and all my level were normal. Except my cholesterol{250} My doctor put Vit D on the script. The level was 72 and the office called and said to take otc 2000 units of Vit D. I am a sun worshiper and find this amusing. Of course I am not going to take this supplement. No one knows the normal level anyway. I went to numerous sites and it ranges from 50 to 70 to over 100. Pharm will get rich over this, better than Fosamax with their bone density crap. I was suckered into that but no more hype for me.
Thank you for sharing this. I've been looking for age related vitamin D information.
Post a Comment