The hypothesis that blood cholesterol levels are positively correlated with heart disease (the lipid hypothesis) dates back to Rudolph Virchow in the mid-1800s.
One famous study that supported this hypothesis was Ancel Keys's Seven Countries Study, conducted between the 1950s and 1970s. This study eventually served as the foundation on which much of the advice that we receive today from doctors is based, even though several other studies have been published since that provide little support for the lipid hypothesis.
The graph below (from O Primitivo) shows the results of one study, involving many more countries than Key's Seven Countries Study, that actually suggests a NEGATIVE linear correlation between total cholesterol and cardiovascular disease.
Now, most relationships in nature are nonlinear, with quite a few following a pattern that looks like a U-curve (plain or inverted); sometimes called a J-curve pattern. The graph below (also from O Primitivo) shows the U-curve relationship between total cholesterol and mortality, with cardiovascular disease mortality indicated through a dotted red line at the bottom.
This graph has been obtained through a nonlinear analysis, and I think it provides a better picture of the relationship between total cholesterol (TC) and mortality. Based on this graph, the best range of TC that one can be at is somewhere between 210, where cardiovascular disease mortality is minimized; and 220, where total mortality is minimized.
The total mortality curve is the one indicated through the full blue line at the top. In fact, it suggests that mortality increases sharply as TC decreases below 200.
Now, these graphs relate TC with disease and mortality, and say nothing about LDL cholesterol (LDL). In my own experience, and that of many people I know, a TC of about 200 will typically be associated with a slightly elevated LDL (e.g., 110 to 150), even if one has a high HDL cholesterol (i.e., greater than 60).
Yet, most people who have a LDL greater than 100 will be told by their doctors, usually with the best of the intentions, to take statins, so that they can "keep their LDL under control". (LDL levels are usually calculated, not measured directly, which itself creates a whole new set of problems.)
Alas, reducing LDL to 100 or less will typically reduce TC below 200. If we go by the graphs above, especially the one showing the U-curves, these folks' risk for cardiovascular disease and mortality will go up - exactly the opposite effect that they and their doctors expected. And that will cost them financially as well, as statin drugs are expensive, in part to pay for all those TV ads.
Saturday, October 22, 2022
Wednesday, July 20, 2022
What is your optimal weight? Maybe it is the one that minimizes your waist-to-weight ratio
There is a significant amount of empirical evidence suggesting that, for a given individual and under normal circumstances, the optimal weight is the one that maximizes the ratio below, where: L = lean body mass, and T = total mass.
L / T
L is difficult and often costly to measure. T can be measured easily, as one’s total weight.
Through some simple algebraic manipulations, you can see below that the ratio above can be rewritten in terms of one’s body fat mass (F).
L / T = (T – F) / T = 1 – F / T
Therefore, in order to maximize L / T, one should maximize 1 – F / T. This essentially means that one should minimize the second term, or the ratio below, which is one’s body fat mass (F) divided by one’s weight (T).
F / T
So, you may say, all I have to do is to minimize my body fat percentage. The problem with this is that body fat percentage is very difficult to measure with precision, and, perhaps more importantly, body fat percentage is associated with lean body mass (and also weight) in a nonlinear way.
In English, it becomes increasingly difficult to retain lean body mass as one's body fat percentage goes down. Mathematically, body fat percentage (F / T) is a nonlinear function of T, where this function has the shape of a J curve.
This is what complicates matters, making the issue somewhat counterintuitive. Six-pack abs may look good, but many people would have to sacrifice too much lean body mass for their own good to get there. Genetics definitely plays a role here, as well as other factors such as age.
Keep in mind that this (i.e., F / T) is a ratio, not an absolute measure. Given this, and to facilitate measurement, we can replace F with a variable that is highly correlated with it, and that captures one or more important dimensions particularly well. This new variable would be a proxy for F. One the most widely used proxies in this type of context is waist circumference. We’ll refer to it as W.
W may well be a very good proxy, because it is a measure that is particularly sensitive to visceral body fat mass, an important dimension of body fat mass. W likely captures variations in visceral body fat mass at the levels where this type of body fat accumulation seems to cause health problems.
Therefore, the ratio that most of us would probably want to minimize is the following, where W is one’s waist circumference, and T is one’s weight.
W / T = waist / weight
Based on the experience of HCE () users, variations in this ratio are likely to be small and require 4-decimals or more to be captured. If you want to avoid having so many decimals, you can multiply the ratio by 1000. This will have no effect on the use of the ratio to find your optimal weight; it is analogous to multiplying a ratio by 100 to express it as a percentage.
Also based on the experience of HCE users, there are fluctuations that make the ratio look like it is changing direction when it is not actually doing that. Many of these fluctuations may be due to measurement error.
If you are obese, as you lose weight through dieting, the waist / weight ratio should go down, because you will be losing more body fat mass than lean body mass, in proportion to your total body mass.
It would arguably be wise to stop losing weight when the waist / weight ratio starts going up, because at that point you will be losing more lean body mass than body fat mass, in proportion to your total body mass.
One’s lowest waist / weight ratio at a given point in time should vary depending on a number of factors, including: diet, exercise, general lifestyle, and age. This lowest ratio will also be dependent on one’s height and genetic makeup.
Mathematically, this lowest ratio is the ratio at which d(W / T) / dT = 0 and d(d(W / T) / dT) / dT > 0. That is, the first derivative of W / T with respect to T equals zero, and the second derivative is greater than zero.
The lowest waist / weight ratio is unique to each individual, and can go up and down over time (e.g., resistance exercise will push it down). Here I am talking about one's lowest waist / weight ratio at a given point in time, not one's waist / weight ratio at a given point in time.
This optimal waist / weight ratio theory is one of the most compatible with evidence regarding the lowest mortality body mass index (, ). Nevertheless, it is another ratio that gets a lot of attention in the health-related literature. I am talking about the waist / hip ratio (). In this literature, waist circumference is often used alone, not as part of a ratio.
Labels:
BMI,
body fat,
body fat loss,
waist-to-weight ratio
Saturday, May 21, 2022
Vitamin D production from UV radiation: The effects of total cholesterol and skin pigmentation
Our body naturally produces as much as 10,000 IU of vitamin D based on a few minutes of sun exposure when the sun is high. Getting that much vitamin D from dietary sources is very difficult, even after “fortification”.
The above refers to pre-sunburn exposure. Sunburn is not associated with increased vitamin D production; it is associated with skin damage and cancer.
Solar ultraviolet (UV) radiation is generally divided into two main types: UVB (wavelength: 280–320 nm) and UVA (320–400 nm). Vitamin D is produced primarily based on UVB radiation. Nevertheless, UVA is much more abundant, amounting to about 90 percent of the sun’s UV radiation.
UVA seems to cause the most skin damage, although there is some debate on this. If this is correct, one would expect skin pigmentation to be our body’s defense primarily against UVA radiation, not UVB radiation. If so, one’s ability to produce vitamin D based on UVB should not go down significantly as one’s skin becomes darker.
Also, vitamin D and cholesterol seem to be closely linked. Some argue that one is produced based on the other; others that they have the same precursor substance(s). Whatever the case may be, if vitamin D and cholesterol are indeed closely linked, one would expect low cholesterol levels to be associated with low vitamin D production based on sunlight.
Bogh et al. (2010) published a very interesting study; one of those studies that remain relevant as time goes by. The link to the study was provided by Ted Hutchinson in the comments sections of a another post on vitamin D. The study was published in a refereed journal with a solid reputation, the Journal of Investigative Dermatology.
The study by Bogh et al. (2010) is particularly interesting because it investigates a few issues on which there is a lot of speculation. Among the issues investigated are the effects of total cholesterol and skin pigmentation on the production of vitamin D from UVB radiation.
The figure below depicts the relationship between total cholesterol and vitamin D production based on UVB radiation. Vitamin D production is referred to as “delta 25(OH)D”. The univariate correlation is a fairly high and significant 0.51.
25(OH)D is the abbreviation for calcidiol, a prehormone that is produced in the liver based on vitamin D3 (cholecalciferol), and then converted in the kidneys into calcitriol, which is usually abbreviated as 1,25-(OH)2D3. The latter is the active form of vitamin D.
The table below shows 9 columns; the most relevant ones are the last pair at the right. They are the delta 25(OH)D levels for individuals with dark and fair skin after exposure to the same amount of UVB radiation. The difference in vitamin D production between the two groups is statistically indistinguishable from zero.
So there you have it. According to this study, low total cholesterol seems to be associated with impaired ability to produce vitamin D from UVB radiation. And skin pigmentation appears to have little effect on the amount of vitamin D produced.
The study has a few weaknesses, as do almost all studies. For example, if you take a look at the second pair of columns from the right on the table above, you’ll notice that the baseline 25(OH)D is lower for individuals with dark skin. The difference was just short of being significant at the 0.05 level.
What is the problem with that? Well, one of the findings of the study was that lower baseline 25(OH)D levels were significantly associated with higher delta 25(OH)D levels. Still, the baseline difference does not seem to be large enough to fully explain the lack of difference in delta 25(OH)D levels for individuals with dark and fair skin.
A widely cited dermatology researcher, Antony Young, published an invited commentary on this study in the same journal issue (Young, 2010). The commentary points out some weaknesses in the study, but is generally favorable. The weaknesses include the use of small sub-samples.
References
Bogh, M.K.B., Schmedes, A.V., Philipsen, P.A., Thieden, E., & Wulf, H.C. (2010). Vitamin D production after UVB exposure depends on baseline vitamin D and total cholesterol but not on skin pigmentation. Journal of Investigative Dermatology, 130(2), 546–553.
Young, A.R. (2010). Some light on the photobiology of vitamin D. Journal of Investigative Dermatology, 130(2), 346–348.
The above refers to pre-sunburn exposure. Sunburn is not associated with increased vitamin D production; it is associated with skin damage and cancer.
Solar ultraviolet (UV) radiation is generally divided into two main types: UVB (wavelength: 280–320 nm) and UVA (320–400 nm). Vitamin D is produced primarily based on UVB radiation. Nevertheless, UVA is much more abundant, amounting to about 90 percent of the sun’s UV radiation.
UVA seems to cause the most skin damage, although there is some debate on this. If this is correct, one would expect skin pigmentation to be our body’s defense primarily against UVA radiation, not UVB radiation. If so, one’s ability to produce vitamin D based on UVB should not go down significantly as one’s skin becomes darker.
Also, vitamin D and cholesterol seem to be closely linked. Some argue that one is produced based on the other; others that they have the same precursor substance(s). Whatever the case may be, if vitamin D and cholesterol are indeed closely linked, one would expect low cholesterol levels to be associated with low vitamin D production based on sunlight.
Bogh et al. (2010) published a very interesting study; one of those studies that remain relevant as time goes by. The link to the study was provided by Ted Hutchinson in the comments sections of a another post on vitamin D. The study was published in a refereed journal with a solid reputation, the Journal of Investigative Dermatology.
The study by Bogh et al. (2010) is particularly interesting because it investigates a few issues on which there is a lot of speculation. Among the issues investigated are the effects of total cholesterol and skin pigmentation on the production of vitamin D from UVB radiation.
The figure below depicts the relationship between total cholesterol and vitamin D production based on UVB radiation. Vitamin D production is referred to as “delta 25(OH)D”. The univariate correlation is a fairly high and significant 0.51.
25(OH)D is the abbreviation for calcidiol, a prehormone that is produced in the liver based on vitamin D3 (cholecalciferol), and then converted in the kidneys into calcitriol, which is usually abbreviated as 1,25-(OH)2D3. The latter is the active form of vitamin D.
The table below shows 9 columns; the most relevant ones are the last pair at the right. They are the delta 25(OH)D levels for individuals with dark and fair skin after exposure to the same amount of UVB radiation. The difference in vitamin D production between the two groups is statistically indistinguishable from zero.
So there you have it. According to this study, low total cholesterol seems to be associated with impaired ability to produce vitamin D from UVB radiation. And skin pigmentation appears to have little effect on the amount of vitamin D produced.
The study has a few weaknesses, as do almost all studies. For example, if you take a look at the second pair of columns from the right on the table above, you’ll notice that the baseline 25(OH)D is lower for individuals with dark skin. The difference was just short of being significant at the 0.05 level.
What is the problem with that? Well, one of the findings of the study was that lower baseline 25(OH)D levels were significantly associated with higher delta 25(OH)D levels. Still, the baseline difference does not seem to be large enough to fully explain the lack of difference in delta 25(OH)D levels for individuals with dark and fair skin.
A widely cited dermatology researcher, Antony Young, published an invited commentary on this study in the same journal issue (Young, 2010). The commentary points out some weaknesses in the study, but is generally favorable. The weaknesses include the use of small sub-samples.
References
Bogh, M.K.B., Schmedes, A.V., Philipsen, P.A., Thieden, E., & Wulf, H.C. (2010). Vitamin D production after UVB exposure depends on baseline vitamin D and total cholesterol but not on skin pigmentation. Journal of Investigative Dermatology, 130(2), 546–553.
Young, A.R. (2010). Some light on the photobiology of vitamin D. Journal of Investigative Dermatology, 130(2), 346–348.
Labels:
cholesterol,
research,
skin pigmentation,
UVA,
UVB,
vitamin D
Sunday, March 20, 2022
Heavy physical activity may significantly reduce heart disease deaths, especially after age 45
The idea that heavy physical activity is a main trigger of heart attacks is widespread. Often endurance running and cardio-type activities are singled out. Some people refer to this as “death by running”. Others think that strength training has a higher lethal potential. We know based on the Oregon Sudden Unexpected Death Study that this is a myth ().
Here is some evidence that heavy physical activity in fact has a significant protective effect. The graph below shows the number of deaths from coronary heart disease, organized by age group, in longshoremen (dock workers). The shaded bars represent those whose level of activity at work was considered heavy. The unshaded bars represent those whose level of activity at work was considered moderate or light (essentially below the “heavy” level).
The data is based on an old and classic study of 6351 men, aged 35 to 74 years, who were followed either for 22 years, or to death, or to the age of 75. It shows a significant protective effect of heavy activity, especially after age 45 () . The numbers atop the unshaded bars reflect the relative risk of death from coronary heart disease in each age group. For example, in the age group 65-74, the risk among those not in the heavy activity group is 110 percent higher (2.1 times higher) than in the heavy activity group.
It should be noted that this is a cumulative effect, of years of heavy activity. Based on the description of the types of activities performed, and the calories spent, I estimate that the heavy activity group performed the equivalent of a few hours of strength training per week, plus a lot of walking and other light physical activities. The authors of the study concluded that “… repeated bursts of high energy output established a plateau of protection against coronary mortality.”
Heavy physical activity may not make you lose much weight, but has the potential to make you live longer.
Saturday, January 22, 2022
Insulin responses to foods rich in carbohydrates and protein
Insulin is often presented as a hormone that is at the core of the diseases of civilization, particularly because of the insulin response elicited by foods rich in refined carbohydrates and sugars. What is often not mentioned is that protein also elicits an insulin response and so do foods where carbohydrates are mixed with fat. Sometimes the insulin responses are way more than one would expect based on the macronutrient compositions of the foods.
Holt et al. (1997; full reference at the end of this post) conducted a classic study of insulin responses. This study has been widely cited, and paints an interesting picture of differences in insulin responses to various foods. But you have to be careful where you look. There has been some confusion about the results because of the way they are often reported in places like Wikipedia and on various Internet sites that refer to the study.
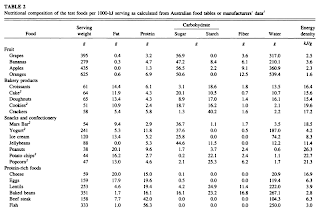
The key thing to bear in mind when reviewing this study is that the amounts of food used were designed to have the same calorie content: 1000 kJ or 240 kcal (i.e., 240 calories). This led to wild variations in the size of the portions that are compared and their weight in grams. Also, some of the food portions are probably not what people usually eat in one sitting.
In Holt et al.’s (1997) study the participants were 41 lean and healthy university students. They were fed 1000 kJ (240 kcal) portions of the test foods on separate mornings after a 10-hour fast overnight. Blood insulin levels were measured at different times within a 120-minute period after each meal. An insulin score was then calculated from the area under the insulin response curve for each food; white bread was used as the reference food.
Part of Table 2 on page 1267 is shown below (the full text version of the paper is linked at the end of this post), just to illustrate the types and amounts of food served, and the macronutrient breakdown for each food. I hope you can see what I meant when I said that some of the food portions are probably not what people usually eat in one sitting. I don’t think it would be hard to find someone who would eat 158 g of beef steak in one sitting, but 333 g of fish is a little more difficult. Fish has a higher proportion of protein than beef steak, and thus is more satiating. The same goes for 625 g of orange, about 6 oranges. Foods that have more fat have more calories per gram; hence the smaller portions served for high-fat foods.
Table 4 of the article is a bit long, so I am providing it in two parts below. AUC stands for “area under the curve”. As you can see, for isocaloric portions of different foods (i.e., with the same amount of calories), there is a huge variation in insulin response. The insulin AUCs are shown on the second numeric column from the left. Also note that the insulin responses (AUC) for white bread varied in different meals. This complicates things a bit, but at least provides a more realistic view of the responses since each participant served as his or her own control.
Look at the third column from the right, which shows the insulin responses per gram of each food, compared with the response to white bread, always shown at the top for each group of related foods (e.g., protein-rich foods). The gram-adjusted response for whole-meal bread is rather high, and so is the glucose response. The gram-adjusted insulin response to potatoes is less than one-third of the response to white bread, even though the non-gram-adjusted glucose response is higher. The insulin response to beef is also less than one-third of the response to white bread, gram-for-gram. Even cheese leads to a gram-adjusted response that is about half the one for white bread, and I don’t think many people will eat the same amount of cheese in one sitting as they would do with white bread.
In summary, insulin responses to protein-rich foods are often 50 to 70 percent lower than responses to equivalent amounts of refined carbohydrate-rich foods. Also, insulin responses to unrefined carbohydrate-rich foods (e.g., potato, fruits) are often 70 to 90 percent lower than responses to equivalent amounts of refined carbohydrate-rich foods.
Why do insulin levels go up in response to dietary protein?
One of the reasons is that insulin is needed for tissue protein synthesis. That is, increased circulating protein (as amino acids) and insulin have a net anabolic effect, promoting muscle growth and inhibiting muscle breakdown. (Muscle protein synthesis and breakdown happen all the time; the net effect defines whether muscle grows or shrinks.) In this respect, insulin acts in conjunction with other hormones, such as growth hormone and insulin-like growth factor 1.
Reference:
Holt, S.H., Miller, J.C., & Petocz, P. (1997). An insulin index of foods: The insulin demand generated by 1000-kJ portions of common foods. American Journal of Clinical Nutrition, 66, 1264-1276.
Holt et al. (1997; full reference at the end of this post) conducted a classic study of insulin responses. This study has been widely cited, and paints an interesting picture of differences in insulin responses to various foods. But you have to be careful where you look. There has been some confusion about the results because of the way they are often reported in places like Wikipedia and on various Internet sites that refer to the study.
The key thing to bear in mind when reviewing this study is that the amounts of food used were designed to have the same calorie content: 1000 kJ or 240 kcal (i.e., 240 calories). This led to wild variations in the size of the portions that are compared and their weight in grams. Also, some of the food portions are probably not what people usually eat in one sitting.
In Holt et al.’s (1997) study the participants were 41 lean and healthy university students. They were fed 1000 kJ (240 kcal) portions of the test foods on separate mornings after a 10-hour fast overnight. Blood insulin levels were measured at different times within a 120-minute period after each meal. An insulin score was then calculated from the area under the insulin response curve for each food; white bread was used as the reference food.
Part of Table 2 on page 1267 is shown below (the full text version of the paper is linked at the end of this post), just to illustrate the types and amounts of food served, and the macronutrient breakdown for each food. I hope you can see what I meant when I said that some of the food portions are probably not what people usually eat in one sitting. I don’t think it would be hard to find someone who would eat 158 g of beef steak in one sitting, but 333 g of fish is a little more difficult. Fish has a higher proportion of protein than beef steak, and thus is more satiating. The same goes for 625 g of orange, about 6 oranges. Foods that have more fat have more calories per gram; hence the smaller portions served for high-fat foods.
Table 4 of the article is a bit long, so I am providing it in two parts below. AUC stands for “area under the curve”. As you can see, for isocaloric portions of different foods (i.e., with the same amount of calories), there is a huge variation in insulin response. The insulin AUCs are shown on the second numeric column from the left. Also note that the insulin responses (AUC) for white bread varied in different meals. This complicates things a bit, but at least provides a more realistic view of the responses since each participant served as his or her own control.
Look at the third column from the right, which shows the insulin responses per gram of each food, compared with the response to white bread, always shown at the top for each group of related foods (e.g., protein-rich foods). The gram-adjusted response for whole-meal bread is rather high, and so is the glucose response. The gram-adjusted insulin response to potatoes is less than one-third of the response to white bread, even though the non-gram-adjusted glucose response is higher. The insulin response to beef is also less than one-third of the response to white bread, gram-for-gram. Even cheese leads to a gram-adjusted response that is about half the one for white bread, and I don’t think many people will eat the same amount of cheese in one sitting as they would do with white bread.
In summary, insulin responses to protein-rich foods are often 50 to 70 percent lower than responses to equivalent amounts of refined carbohydrate-rich foods. Also, insulin responses to unrefined carbohydrate-rich foods (e.g., potato, fruits) are often 70 to 90 percent lower than responses to equivalent amounts of refined carbohydrate-rich foods.
Why do insulin levels go up in response to dietary protein?
One of the reasons is that insulin is needed for tissue protein synthesis. That is, increased circulating protein (as amino acids) and insulin have a net anabolic effect, promoting muscle growth and inhibiting muscle breakdown. (Muscle protein synthesis and breakdown happen all the time; the net effect defines whether muscle grows or shrinks.) In this respect, insulin acts in conjunction with other hormones, such as growth hormone and insulin-like growth factor 1.
Reference:
Holt, S.H., Miller, J.C., & Petocz, P. (1997). An insulin index of foods: The insulin demand generated by 1000-kJ portions of common foods. American Journal of Clinical Nutrition, 66, 1264-1276.
Subscribe to:
Comments (Atom)