This post refers to an interesting study by Yashin and colleagues (2009) at Duke University’s Center for Population Health and Aging. (The full reference to the article, and a link, are at the end of this post.) This study is a gem with some rough edges, and some interesting implications.
The study uses data from the Framingham Heart Study (FHS). The FHS, which started in the late 1940s, recruited 5209 healthy participants (2336 males and 2873 females), aged 28 to 62, in the town of Framingham, Massachusetts. At the time of Yashin and colleagues’ article publication, there were 993 surviving participants.
I rearranged figure 2 from the Yashin and colleagues article so that the two graphs (for females and males) appeared one beside the other. The result is shown below (click on it to enlarge); the caption at the bottom-right corner refers to both graphs. The figure shows the age-related trajectory of blood glucose levels, grouped by lifespan (LS), starting at age 40.
As you can see from the figure above, blood glucose levels increase with age, even for long-lived individuals (LS > 90). The increases follow a U-curve (a.k.a. J-curve) pattern; the beginning of the right side of a U curve, to be more precise. The main difference in the trajectories of the blood glucose levels is that as lifespan increases, so does the width of the U curve. In other words, in long-lived people, blood glucose increases slowly with age; particularly up to 55 years of age, when it starts increasing more rapidly.
Now, here is one of the rough edges of this study. The authors do not provide standard deviations. You can ignore the error bars around the points on the graph; they are not standard deviations. They are standard errors, which are much lower than the corresponding standard deviations. Standard errors are calculated by dividing the standard deviations by the square root of the sample sizes for each trajectory point (which the authors do not provide either), so they go up with age since progressively smaller numbers of individuals reach advanced ages.
So, no need to worry if your blood glucose levels are higher than those shown on the vertical axes of the graphs. (I will comment more on those numbers below.) Not everybody who lived beyond 90 had a blood glucose of around 80 mg/dl at age 40. I wouldn't be surprised if about 2/3 of the long-lived participants had blood glucose levels in the range of 65 to 95 at that age.
Here is another rough edge. It is pretty clear that the authors’ main independent variable (i.e., health predictor) in this study is average blood glucose, which they refer to simply as “blood glucose”. However, the measure of blood glucose in the FHS is a very rough estimation of average blood glucose, because they measured blood glucose levels at random times during the day. These measurements, when averaged, are closer to fasting blood glucose levels than to average blood glucose levels.
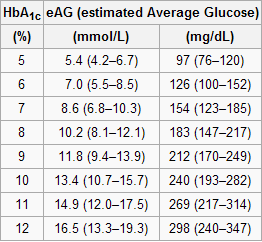
A more reliable measure of average blood glucose levels is that of glycated hemoglobin (HbA1c). Blood glucose glycates (i.e., sticks to, like most sugary substances) hemoglobin, a protein found in red blood cells. Since red blood cells are relatively long-lived, with a turnover of about 3 months, HbA1c (given in percentages) is a good indicator of average blood glucose levels (if you don’t suffer from anemia or a few other blood abnormalities). Based on HbA1c, one can then estimate his or her average blood glucose level for the previous 3 months before the test, using one of the following equations, depending on whether the measurement is in mg/dl or mmol/l.
Average blood glucose (mg/dl) = 28.7 × HbA1c − 46.7
Average blood glucose (mmol/l) = 1.59 × HbA1c − 2.59
The table below, from Wikipedia, shows average blood glucose levels corresponding to various HbA1c values. As you can see, they are generally higher than the corresponding fasting blood glucose levels would normally be (the latter is what the values on the vertical axes of the graphs above from Yashin and colleagues’ study roughly measure). This is to be expected, because blood glucose levels vary a lot during the day, and are often transitorily high in response to food intake and fluctuations in various hormones. Growth hormone, cortisol and noradrenaline are examples of hormones that increase blood glucose. Only one hormone effectively decreases blood glucose levels, insulin, by stimulating glucose uptake and storage as glycogen and fat.
Nevertheless, one can reasonably expect fasting blood glucose levels to have been highly correlated with average blood glucose levels in the sample. So, in my opinion, the graphs above showing age-related blood glucose trajectories are still valid, in terms of their overall shape, but the values on the vertical axes should have been measured differently, perhaps using the formulas above.
Ironically, those who achieve low average blood glucose levels (measured based on HbA1c) by adopting a low carbohydrate diet (one of the most effective ways) frequently have somewhat high fasting blood glucose levels because of physiological (or benign) insulin resistance. Their body is primed to burn fat for energy, not glucose. Thus when growth hormone levels spike in the morning, so do blood glucose levels, as muscle cells are in glucose rejection mode. This is a benign version of the dawn effect (a.k.a. dawn phenomenon), which happens with quite a few low carbohydrate dieters, particularly with those who are deep in ketosis at dawn.
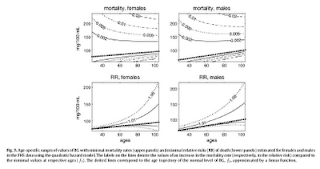
Yashin and colleagues also modeled relative risk of death based on blood glucose levels, using a fairly sophisticated mathematical model that takes into consideration U-curve relationships. What they found is intuitively appealing, and is illustrated by the two graphs at the bottom of the figure below. The graphs show how the relative risks (e.g., 1.05, on the topmost dashed line on the both graphs) associated with various ranges of blood glucose levels vary with age, for both females and males.
What the graphs above are telling us is that once you reach old age, controlling for blood sugar levels is not as effective as doing it earlier, because you are more likely to die from what the authors refer to as “other causes”. For example, at the age of 90, having a blood glucose of 150 mg/dl (corrected for the measurement problem noted earlier, this would be perhaps 165 mg/dl, from HbA1c values) is likely to increase your risk of death by only 5 percent. The graphs account for the facts that: (a) blood glucose levels naturally increase with age, and (b) fewer people survive as age progresses. So having that level of blood glucose at age 60 would significantly increase relative risk of death at that age; this is not shown on the graph, but can be inferred.
Here is a final rough edge of this study. From what I could gather from the underlying equations, the relative risks shown above do not account for the effect of high blood glucose levels earlier in life on relative risk of death later in life. This is a problem, even though it does not completely invalidate the conclusion above. As noted by several people (including Gary Taubes in his book Good Calories, Bad Calories), many of the diseases associated with high blood sugar levels (e.g., cancer) often take as much as 20 years of high blood sugar levels to develop. So the relative risks shown above underestimate the effect of high blood glucose levels earlier in life.
Do the long-lived participants have some natural protection against accelerated increases in blood sugar levels, or was it their diet and lifestyle that protected them? This question cannot be answered based on the study.
Assuming that their diet and lifestyle protected them, it is reasonable to argue that: (a) if you start controlling your average blood sugar levels well before you reach the age of 55, you may significantly increase your chances of living beyond the age of 90; (b) it is likely that your blood glucose levels will go up with age, but if you can manage to slow down that progression, you will increase your chances of living a longer and healthier life; (c) you should focus your control on reliable measures of average blood glucose levels, such as HbA1c, not fasting blood glucose levels (postprandial glucose levels are also a good option, because they contribute a lot to HbA1c increases); and (d) it is never too late to start controlling your blood glucose levels, but the more you wait, the bigger is the risk.
References:
Taubes, G. (2007). Good calories, bad calories: Challenging the conventional wisdom on diet, weight control, and disease. New York, NY: Alfred A. Knopf.
Yashin, A.I., Ukraintseva, S.V., Arbeev, K.G., Akushevich, I., Arbeeva, L.S., & Kulminski, A.M. (2009). Maintaining physiological state for exceptional survival: What is the normal level of blood glucose and does it change with age? Mechanisms of Ageing and Development, 130(9), 611-618.
Tuesday, June 22, 2021
Subscribe to:
Post Comments (Atom)


15 comments:
An interesting post on blood sugar levels and control as a predictor of longevity.
Quite by chance, the following link
http://www.telegraph.co.uk/health/healthnews/7634178/An-unhealthy-lifestyle-makes-you-12-years-older.html
suggests that eliminating smoking, drinking too much,lack of exercise and poor diet increases longevity also.
I am struck by two thoughts:
1) do these items have any correlation with blood sugar
2) may we construct a measure of physiological age based on blood sugar level?
Thank you for this post
Very interesting I've become a bit of a freak for testing my glucose response to various foods. This reminds me why.
Hi Leon. Interesting article. These things happen slowly indeed. I think blood sugar is a marker for something else, a more fundamental metabolic disorder. Those factors, with the possible exception of smoking, are probably all causally linked with the same fundamental metabolic disorder.
Hi Tom. Thanks for stopping by.
Hi Ned,
So, does it mean anything if as a low carber I don't have high fasting blood glucose in the morning?
Hi lightcan.
I don't think it means anything bad. Not everybody on a low carb diet experience that effect.
It seems that the effect is somewhat associated with ketonuria (ketones in the urine) in the morning.
So, if you don't experience ketonuria, that may be the reason. Mild ketonuria will usually be indicated on standard urine test reports.
But not everybody experiencing ketonuria also experience elevated fasting blood glucose levels.
Thanks Ned,
can you tell me if you have a discussion of HbA1c on your blog, sorry, I don't have the time now to do the research. What are the factors that might influence it, is it reliable as an indicator of average glucose levels? Should I try Jenny's blog?
Thanks.
Last time I checked mine was 5.2 and I understand that lower could be better. But seeing your last post that contains an analysis blood glucose of 'normal' people on a 'normal' diet and have a similar average HbA1c to mine, on a low carb diet, raises some questions.
HbA1c seems reasonably reliable, unless you have one of a few, not very common, blood abnormalities, such as anemia. I say reliable in the sense that it does not give as many false positives as other measures, such as fasting blood glucose levels.
But HbA1c is not very precise. As you can see from the table on this post, a level of 5% corresponds to an average blood glucose of 76 to 120 (quite a range).
Bear in mind that there are a number of factors that may increase your blood glucose levels. Diet is one of them - usually the most important. Stress is also one of them, via the action of stress hormones.
This is totally anecdotal, but I have seen some cases that suggest that severe calorie restriction may increase average blood glucose while weight loss is happening, because of excess circulating stress hormones. Once you reach a plateau of weight and keeps it for a while (a few weeks; not need to gain any weight back, just to keep it stable for a while), the normal hormonal balance is re-established and blood glucose levels fall.
Hi Ned,
If you are eating 50-75 g of carbs per day, do you think it would be better to eat all your carbs in one meal or to spread them out over two or even three meals?
Hi Monty.
I think it would make sense to spread the intake, and eat the carbs with other foods containing fat, protein.
Fat in particular seems to blunt the glucose response to any food.
Re: Ironically, those who achieve low average blood glucose levels (measured based on HbA1c) by adopting a low carbohydrate diet (one of the most effective ways) frequently have somewhat high fasting blood glucose levels because of physiological (or benign) insulin resistance. Their body is primed to burn fat for energy, not glucose. Thus when growth hormone levels spike in the morning, so do blood glucose levels, as muscle cells are in glucose rejection mode. This is a benign version of the dawn effect (a.k.a. dawn phenomenon), which happens with quite a few low carbohydrate dieters, particularly with those who are deep in ketosis at dawn."
Wish I had read that again before checking my BG for the first time Sunday morning just after arising, Ned. 134!!! I freaked out. Today it was 122. Then it normalizes around 106. I'll be 70 in Oct, so I'm not too concerned now. But, man, I was for a couple of days before reading about the dawn effect. Also enjoyed/profited from your most recent post related to this topic.
Thanks!
Hi Jim.
Interestingly, some people go on a high carb diet (including refined carbs like cereals) and see a decrease in the FBG. They are happy, until they get a measure of average blood glucose done and realize that it is too high.
Their FBG goes down with HC because they are not as sensitive to carbs anymore. Still, their postprandial levels (which they don't measure) and going through the roof. And research suggests that it is primarily the postprandial levels that should be controlled in normoglycemics:
http://healthcorrelator.blogspot.com/2010/05/postprandial-glucose-levels-hba1c-and.html
Here is a comment from reader Marc, via email:
"At the end of section 2.1 the authors state that for all of their analyses they determined blood glucose using whole blood (rather than make you search for the article in your old files, I'm attaching a copy). If I understand that sentence correctly, that would mean that all of the figures in their tables are considerably lower than they would be if the measurements had been made using plasma glucose levels."
Thanks much Marc. Here is part of my response:
"You are absolutely right. The conversion rate is 1.15 or something like that, if I'm not mistaken.
[...] this topic requires a full post, because it also has some bearing on the interpretation of new blood glucose results vis-à-vis results obtained in the old days."
What do you think of adding starches back in such as suggested in The Perfect Health Diet if your A1C is 5.9, but got lowered to 5.5 with avoiding starches?
My goal is to lower that A1C but I hear so much about adding potatoes back in. My fasting sugars are great and my post prandials are good too. I have tested after eating a sweet potato, rice or potato and the sugars to go up. Any ideas?
Have you try any natural supplement or medicine for Control high blood sugar.
Thanks for your post also thanks for that your giving us great information for living beyond 90. Please keep posting.
This post is a further revised version of a previous post. The original comments are preserved here. More comments welcome, but no spam please!
Post a Comment