This is a study (Grieb, P. et al., 2008; full reference at the end of this post) that I read a few years ago, right after it came out, and at the time I recall thinking about the apparent contradiction between the positive effects of the Optimal Diet and the very elevated LDL cholesterol levels among the participants. I say “contradiction” because of the established and misguided dogma among medical doctors, particularly general practitioners, that decreasing LDL cholesterol levels is the best strategy to avoid cardiovascular disease.
The Optimal Diet is one of the best examples of a healthy diet where LDL cholesterol levels are generally high, in fact much higher than most people are willing to accept as healthy today. (In this study, LDL cholesterol levels were calculated based on the Friedewald equation.)
It is not uncommon to see people concerned about their high LDL cholesterol levels after adopting a low carbohydrate diet. (A low carbohydrate diet is, generally speaking, a high fat diet.) This study shows that this is a rather common thing, and also that it is not something that those who experience it should be too concerned about. To be convinced of this, one can always do a VAP test (see this post for a link to a sample VAP test report) and check his or her LDL particle pattern.
The study presents the Optimal Diet as the Polish equivalent to the Atkins diet. It states that the Diet’s main characteristic is maintaining the proportion of proteins:fat:carbs. in the range of 1:2.5-3.5:0.5, with no restriction on the amount of food consumed. In fact, as you will see in this post, more than 70 percent of the calories consumed by the study participants came from fat.
Easily digestible carbohydrate-rich foods are not part of the Optimal Diet. More specifically, the following foods were listed as not being allowed in the Optimal Diet: sucrose, sweets, honey, jam, white rice, bread, starches in general, beans, potatoes (only in small amounts), and sweetened drinks. Also, the Optimal Diet is definitely a low carbohydrate diet, but not what is often referred to as a "very low carbohydrate diet". In this study, the typical carbohydrate intake per day was around 60 g.
Thirty-one healthy people participated in the study, 17 women and 14 men. The average age was 51.7 (standard deviation: 16.6). They had self-reportedly adhered to the Optimal Diet for at least 1 year prior to the study; the average period of adherence was 4.1 years (standard deviation: 1.9). So, the vast majority had been on the diet for more than 2.2 years, about half for 4.1 years or more, and about one-sixth for more than 6 years. (Check this post if you want to know how these figures can be calculated based on the average period of adherence and the standard deviation.)
The table below (click on it to enlarge) shows anthropometric and physiologic characteristics of the participants. Note that longer adherence to the Optimal Diet (right end of the table) was associated with lower systolic and diastolic blood pressure, as well as lower body mass index (BMI). (It was also associated with lower height and BMR, so I am guessing that more women tended to be long-term adherers than men.) Most of the participants had BMIs in the normal range, with only one in the obese category. That was a 43-year-old man who followed the diet for 1.5 years; he had a BMI of 34.1.
The macronutrient distribution of the Optimal Diet is shown on the table below (click on it to enlarge), as followed by the participants. As you can see, protein intake was not that high; about 53.9 g per day on average for men, a bit less for women. Note the percentage of calories from fat: more than 77 percent for men and 72 percent for women. Given the BMIs just discussed, one can safely say based on this that eating a lot of fat did not make the participants fat.
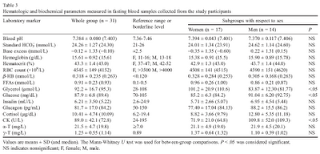
The table below (click on it to enlarge) has some interesting health markers. Note that free fatty acids (FFAs) were elevated. This is to be expected, as these folks were burning fat for energy most of the time, and not as much glucose. The FFAs are not really “free”, but bound to a protein called albumin, which is abundant in human blood. FFAs yield large quantities of adenosine triphosphate (ATP), the main energy “currency” used by the body.
These levels of FFAs are also usually associated with mild ketosis, where ketones are produced by the body and used for energy. Unlike albumin-bound FFAs, ketones are soluble in water, and thus circulate freely through the blood. The mild ketosis experienced by the participants was possibly to the point where ketones showed in the urine. The article mentions this, and provides a measure of beta-HB (beta-hydroxybutyrate, a ketone body), which is elevated as expected, but does not provide urine or other blood ketone measures (e.g., blood acetone levels). Also note the fairly healthy fasting glucose levels, slightly higher in men than in women, but fairly low overall. Fairly healthy insulin levels as well; at the high end of what Stephan at Whole Health Source would recommend, but still significantly lower than the average insulin level in the U.S. at the time of the article's publication.
Finally, the table below (click on it to enlarge) shows lipids and a few other measures. Total cholesterol was on average a bit more than 278 mg/dL. LDL cholesterol was a bit higher than 188 mg/dL on average; high enough to make most doctors cringe today. Based on the means and standard deviations provided, we can estimate that about 16 percent of the participants had LDL cholesterol levels higher than 228.1 mg/dL. About 2.5 percent of the participants had LDL cholesterol levels higher than 268 mg/dL. And this is all after adhering to the diet for a relatively long period of time; even higher LDL cholesterol levels might have occurred right after adoption.
Yet average HDL cholesterol was a very high and protective 71.6 mg/dL. This high HDL and the relatively low triglycerides suggest a large-buoyant non-atherogenic LDL particle pattern.
Average HOMA(IR), a measure of insulin resistance, was a low 1.35 mU/mmol; strongly indicating, together with the relatively low fasting glucose levels, that the participants were far from being pre-diabetic, let alone diabetic.
Diabetes is a strong risk factor for cardiovascular disease, and many other health complications; much more so than elevated LDL cholesterol.
The Optimal Diet does not seem to be a diet for bodybuilders, but I would say that, overall, Peter at Hyperlipid has chosen a diet that makes some sense.
Reference:
Grieb, P. et al. (2008). Long-term consumption of a carbohydrate-restricted diet does not induce deleterious metabolic effects. Nutrition Research, 28(12), 825-833.
Tuesday, April 13, 2010
Subscribe to:
Post Comments (Atom)




13 comments:
Thanks for the interesting article.
As a former LC for 12 years I´m on keto for
over 6 months now. Everything by trial and error and some scientific research just to feel confirmed. At the end there are always facts which counts: HDL 200, Triglyceride 35, BMI 20, skyrocking D3; asthma and atopic issues vanished, mood rollercoaster normalized, binge attacks away and for sure there is a lot more. Each should find its own optimal way.
Hi Byron.
I agree, we are all similar and different at the same time.
A 200 HDL! That's the highest I've ever heard!
I just found your blog after reading your comment on vitamin D on Dr Davis's heartscanblog. This post on cholesterol interested me greatly as I have been on a low carb diet for three years now and my cholesterol levels climb and climb and are very similar to this study ! Last one at the end of March was total cholesterol 274, HDL 104, LDL 162 and triglycerides 44. I was a little concerned about the LDL whereupon my endocrinologist commented 'it's only a calculated value" :-) I recalculated my LDL using a modified Friedewald formula http://www.ams.ac.ir/aim/08113/0014.htm (The Impact of Low Serum Triglyceride on LDL-Cholesterol Estimation) and my new calculated LDL is 119.
Either way, new formula or old I'm happy. And my vitamin D levels are very good too, in the range of 60 ng/ml to 80 ng/ml on only 2000 IU D3 per day in a northern latitude (UK) but I eat oily fish every day.
Hi Anne.
Your numbers look very good. I calculated your LDL using those numbers, and got around the same LDL as you did using the Iranian equation:
http://healthcorrelator.blogspot.com/2010/04/friedewald-and-iranian-equations.html
And, there is more, if you do a VAP test (where LDL is measured directly) I bet you will be told that you have LDL particles of Pattern A:
http://healthcorrelator.blogspot.com/2010/04/low-fasting-triglycerides-marker-for.html
Pattern A is nonatherogenic, because large LDL particles (>= 26 nm) cannot penetrate the gaps in the endothelium to create plaque.
@ javier: No spam please.
Ned,
Wow! what an informative and comforting blog! I've worried myself to death in the past because of my very high genetic LDL-C (average 228). It seems like there is so much conflicting evidence, I never know if I should take a statin or not.
Since what you are saying makes so much more sense,I have a few questions for you since it seems that most doctors are very unfamiliar with lipoprotein testing and the latest research.
1. If only small, dense LDL-P can penetrate the endothelium, doesn't the high CAD risk that accompanies FH hypercholesterolemia negate this assertion?
2. In your opinion, does a high LDL particle number in and of itself, correlate with a higher chance of CAD, or is that only the case when the LDL-P are small and dense?
Hi Davide, thanks.
My knowledge is only as good as the articles I have reviewed for the posts. And I haven't reviewed any article specifically on FH yet.
It seems to me that FH is rare and related to a genetic mutation that affects the LDL receptor protein. It is also my impression that many people are told that they have FH, when in fact they don't. Their elevated LDL is caused by other factors; an unhealthy diet being one of them.
When we talk about CAD, LDL particle size seems to be one part of the equation, another is inflammation, and there may be several others. Folks who truly have FH are in a special category, and statins may be advisable for them.
Based on my research I think that, generally, having a high proportion of small-dense LDL particles significantly predisposes one to CAD.
Have you ever done a VAP test?
Yeah, I assume that I have a mild case of FH hypercholesterolemia because diet does very little to affect my LDL-C. Also, the vast majority of my LDL-P are very large whether I watch my sugar intake or not (consistent with FH).
FYI, I have taken a lipoprotein test, and when I avoid sugar/refined carbs, I have 97% large LDL-P.
My point, however, was this: You seemed to suggest that only small, dense LDL-P are atherogenic. However, most FH constituents naturally do not have a high percentage of small dense LDL-p and still are predisposed to a high risk of CAD.
Perhaps if the LDL-P is high enough, large LDL-P are still able to penetrate the endothelium. ?
Hi Davide.
Based on what I know about FH, I would speculate that the problem is one of clearance speed. That is, in FH the LDL particles don't get recycled as they would normally be, within a few days.
Given that, LDL particles stay longer in circulation. Even if one has a small proportion of sd-LDL particles, those sd-LDL particles will do damage if they are not cleared soon enough. In the long run, damage accumulates.
Statins have an effect on the receptors, so I have to assume that they can be helpful in cases of FH.
I can also speculate that postprandial glucose management is critical for folks with FH, because high postprandial glucose leads to enhanced glycation, which increases the atherogenic potential of the long-lived sd-LDL.
It also makes sense for folks with FH, I think, to try to ensure that LDL particles are mostly large and buoyant.
So, in summary, I don't think the lb-LDL particles are the problem. The problem is the relatively small number of sd-LDL particles that are not cleared quickly enough. If they are not cleared as quickly as they should, they become a much better target for glycation and oxidation.
Nad,
You make a very interesting point, that I never considered:
Small, dense LDL-P have have a very low affinity to LDL receptors--they circulate in the blood a lot longer than large LDL-P (average 3-4 days). Thus, they are prone to oxidation and are highly atherogenic.
Since FH constituents already have very few LDL receptors, then that would mean that their small LDL-p would circulate even longer! Their small LDL-p is even more dangerous! I'm conjecturing, but perhaps this extra circulation time means a much higher ratio of oxidized, small LDL particles lodging in the endothelium.
If this notion were correct, then that would mean that even average numbers of small LDL-p are very dangerous for FH patients--much more dangerous compared to someone with a normal amount LDL-receptors.
Hi Davide.
Another front on which to attack the problem is increasing your HDL, if you have not done that already. The following posts (the first one, in particular) may be useful in that respect:
http://healthcorrelator.blogspot.com/2010/02/what-should-be-my-hdl-cholesterol.html
http://healthcorrelator.blogspot.com/2010/02/large-ldl-and-small-hdl-particles-best.html
That is quite a good study. Optimal diet sure looks very promising.
Post a Comment